Productive strategy in binary options 60 sec
Diabetes mellitus is a complex, chronic illness requiring continuous medical care with multifactorial risk reduction strategies beyond glycemic control. Ongoing patient self-management education and support are critical to preventing acute complications and reducing the risk of long-term complications. Significant evidence exists that supports a range of interventions to improve diabetes outcomes. The Standards of Care recommendations are not intended to preclude clinical judgment and must be applied in the context of excellent clinical care and with adjustments for individual preferences, comorbidities, and other patient factors.
For more detailed information about management of diabetes, refer to references 12. The recommendations include screening, diagnostic, and therapeutic actions that are known or believed to favorably affect health outcomes of patients with diabetes. Many of these interventions have also been shown to be cost-effective 3.
A grading system Table 1 developed by ADA and modeled after existing methods was used to clarify and codify the evidence that forms the basis for the recommendations. The letters ABCor E show the evidence level that supports each recommendation. The Standards of Care conclude with evidence and recommendations for strategies to improve the process of diabetes care. Type 2 diabetes due to a progressive insulin secretory defect on the background of insulin resistance.
Other specific types of diabetes due to other causes, e. Gestational diabetes mellitus GDM diabetes diagnosed during pregnancy that is not clearly overt diabetes.
Some patients cannot be clearly classified as type 1 or type 2 diabetic. Clinical presentation and disease progression vary considerably in both types of diabetes. Occasionally, patients diagnosed with type 2 diabetes may present with ketoacidosis.
However, difficulties in diagnosis may occur in children, adolescents, and adults, with the true diagnosis becoming more obvious over time. Diabetes is usually diagnosed based on plasma glucose criteria, either the fasting plasma glucose FPG or the 2-h plasma glucose 2-h PG value after a g oral glucose tolerance test OGTT 4.
The A1C test should be performed using a method that is certified by the National Glycohemoglobin Standardization Program NGSP and standardized or traceable to the Diabetes Control and Complications Trial DCCT reference assay. Although point-of-care POC A1C assays may be NGSP-certified, proficiency testing is not mandated for performing the test, so use of these assays for diagnostic purposes may be problematic. Epidemiological data show a similar relationship of A1C with the risk of retinopathy as seen with FPG and 2-h PG.
The A1C has several advantages to the FPG and OGTT, including greater convenience fasting not requiredpossibly greater preanalytical stability, and less day-to-day perturbations during stress and illness.
These advantages must be balanced by greater cost, the limited availability of A1C testing in certain regions of the developing world, and the incomplete correlation between A1C and average glucose in certain individuals. Glycation rates may differ by race. For example, African Americans may have higher rates of glycation, but this is controversial.
A recent epidemiological study found that, when matched for FPG, African Americans with and without diabetes had higher A1C than non-Hispanic whites, but also had higher levels of fructosamine and glycated albumin and lower levels of 1,5 anhydroglucitol, suggesting that their glycemic burden particularly postprandially may be higher 8. Epidemiological studies forming the framework for recommending A1C to diagnose diabetes have all been in adult populations. It is unclear if the same A1C cut point should be used to diagnose children or adolescents with diabetes 9 Interpreting A1C levels in the presence of certain anemias and hemoglobinopathies is particularly problematic.
For patients with an abnormal hemoglobin but normal red cell turnover, such as sickle cell trait, an A1C assay without interference from abnormal hemoglobins should be used. An updated list is available at www.
In situations of abnormal red cell turnover, such as pregnancy, recent blood loss or transfusion, or some anemias, only blood glucose criteria should be used to diagnose diabetes. In addition to the A1C test, the FPG and 2-h PG may also be used to diagnose diabetes.
The current diagnostic criteria for diabetes are summarized in Table 2. The concordance between A1C and either glucose-based test is also imperfect. Numerous studies have confirmed that, at these cut points, the 2-h OGTT value diagnoses more screened people with diabetes In reality, a large portion of the diabetic population remains undiagnosed.
As with most diagnostic tests, a test result should be repeated when feasible to rule out laboratory error e. Unless there is a clear clinical diagnosis e.
For example, if the A1C is 7. If two different tests such as A1C and FPG are both above the diagnostic threshold, this also confirms the diagnosis. On the other hand, if a patient has discordant results on two different tests, then the test result that is above the diagnostic cut point should be repeated. The diagnosis is made on the basis of the confirmed test. Since there is preanalytic and analytic variability of all the tests, it is possible that an abnormal result i.
This is least likely for A1C, somewhat more likely for FPG, and most likely for the 2-h PG. Barring a laboratory error, such patients will likely have test results near the margins of the diagnostic threshold. The health care professional might opt to follow the patient closely and repeat the test in 3—6 months. In andthe Expert Committee on Diagnosis and Classification of Diabetes Mellitus 1314 recognized a group of individuals whose glucose levels did not meet the criteria for diabetes, but were too high to be considered normal.
IFG and IGT should not be viewed as clinical entities in their own right but rather risk factors for diabetes and cardiovascular disease CVD. As with the glucose measures, several prospective studies that used A1C to predict the progression to diabetes demonstrated a strong, continuous association between A1C and subsequent diabetes. In a systematic review of 44, individuals from 16 cohort studies with a follow-up interval averaging 5.
An A1C range of 6. In a community-based study of African American and non-Hispanic white adults without diabetes, baseline A1C was a stronger predictor of subsequent diabetes and cardiovascular events than fasting glucose Other analyses suggest that an A1C of 5.
Hence, it is reasonable to consider an A1C range of 5. As with those with IFG and IGT, individuals with an A1C of 5. Similar to glucose measurements, the continuum of risk is curvilinear, so as A1C rises, the diabetes risk rises disproportionately Aggressive interventions and vigilant follow-up should be pursued for those considered at very high risk e.
Table 3 summarizes the categories of prediabetes. In those without these risk factors, testing should begin at age 45 years. If tests are normal, repeat testing at least at 3-year intervals is reasonable. To test for diabetes or prediabetes, the A1C, FPG, or 2-h g OGTT are appropriate. In those identified with prediabetes, identify and, if appropriate, treat other CVD risk factors. Criteria for testing for diabetes in asymptomatic adult individuals.
The same tests are used for both screening and diagnosing diabetes. Diabetes may be identified anywhere along the spectrum of clinical scenarios: The discussion herein is primarily framed as testing for diabetes in asymptomatic individuals. The same assays used for testing will also detect individuals with prediabetes. Prediabetes and diabetes meet established criteria for conditions in which early detection is appropriate.
Both conditions are common, are increasing in prevalence, and impose significant public health burdens. There is often a long presymptomatic phase before the diagnosis of type 2 diabetes is made. Simple tests to detect preclinical disease are readily available. The duration of glycemic burden is a strong predictor of adverse outcomes, and effective interventions exist to prevent progression of prediabetes to diabetes see Section IV and to reduce risk of complications of diabetes see Section VI.
Type 2 diabetes is frequently not diagnosed until complications appear. Approximately one-fourth of the U. Mass screening of asymptomatic individuals has not effectively identified those with prediabetes or diabetes, and rigorous clinical trials to provide such proof are unlikely to occur.
In a large randomized controlled trial RCT in Europe, general practice patients between the ages of 40—69 years were screened for diabetes, then randomized by practice to routine diabetes care or intensive treatment of multiple risk factors.
Incidence of first CVD event and mortality rates were not significantly different between groups This study would seem to add support for early treatment of screen-detected diabetes, as risk factor control was excellent even in the routine treatment arm and both groups had lower event rates than predicted. The absence of a control unscreened arm limits the ability to definitely prove that screening impacts outcomes.
Testing recommendations for diabetes in asymptomatic, undiagnosed adults are listed in Table 4. In addition to the listed risk factors, certain medications, such as glucocorticoids and antipsychotics 20are known to increase the risk of type 2 diabetes.
There is compelling evidence that lower BMI cut points suggest diabetes risk in some racial and ethnic groups. Disparities in screening rates, not explainable by insurance status, are highlighted by evidence that despite much higher prevalence of type 2 diabetes, ethnic minorities in an insured population are no more likely than non-Hispanic whites to be screened for diabetes Because age is a major risk factor for diabetes, in those without these risk factors, testing should begin at age 45 years.
The A1C, FPG, or the 2-h OGTT are appropriate for testing. It should be noted that the tests do not necessarily detect diabetes in the same individuals.
The efficacy of interventions for primary prevention of type 2 diabetes 23 — 29 has primarily been demonstrated among individuals with IGT, not for individuals with isolated IFG or for individuals with specific A1C levels. The appropriate interval between tests is not known The rationale for the 3-year interval is that false negatives will be repeated before substantial time elapses. It is also unlikely that an individual will develop significant complications of diabetes within 3 years of a negative test result.
In the modeling study, repeat screening every 3 or 5 years was cost-effective Testing should be carried out within the health care setting because of the need for follow-up and discussion of abnormal results.
Community screening outside a health care setting is not recommended because people with positive tests may not seek, or have access to, appropriate follow-up testing and care. Conversely, there may be failure to ensure appropriate repeat testing for individuals who test negative. Community screening may also be poorly targeted; i. Testing to detect type 2 diabetes and prediabetes should be considered in children and adolescents who are overweight and who have two or more additional risk factors for diabetes Table 5.
In the last decade, the incidence of type 2 diabetes in adolescents has increased dramatically, especially in minority populations As with adult recommendations, children and youth at increased risk for the presence or the development of type 2 diabetes should be tested within the health care setting Recent studies question the validity of A1C in the pediatric population, especially in ethnic minorities, and suggest OGTT or FPG as more suitable diagnostic tests However, many of these studies do not recognize that diabetes diagnostic criteria are based upon long-term health outcomes, and validations are not currently available in the pediatric population ADA acknowledges the limited data supporting A1C for diagnosing diabetes in children and adolescents.
JAUREGIA ESNEKIAK
However, aside from rare instances, such as cystic fibrosis and hemoglobinopathies, ADA continues to recommend A1C in this cohort 35 Inform type 1 diabetic patients of the opportunity to have their relatives screened for type 1 diabetes risk in the setting of a clinical research study.
Type 1 diabetic patients often present with acute symptoms of diabetes and markedly elevated blood glucose levels, and some cases are diagnosed with life-threatening ketoacidosis. The incidence and prevalence of type 1 diabetes is increasing 3137 Several studies suggest that measuring islet autoantibodies in relatives of those with type 1 diabetes may identify individuals who are at risk for developing type 1 diabetes.
Such testing, coupled with education about diabetes symptoms and close follow-up in an observational clinical study, may enable earlier identification of type 1 diabetes onset.
A recent study reported the risk of progression to type 1 diabetes from the time of seroconversion to autoantibody positivity in three pediatric cohorts from Finland, Germany, and the U. These findings are highly significant because, while the German group was recruited from offspring of parents with type 1 diabetes, the Finnish and Colorado groups were recruited from the general population. There is evidence to suggest that early diagnosis may limit acute complications 39 and extend long-term endogenous insulin production While there is currently a lack of accepted screening programs, one should consider referring relatives of those with type 1 diabetes for antibody testing for risk assessment in the setting of a clinical research study http: Widespread clinical testing of asymptomatic low-risk individuals is not currently recommended.
Higher-risk individuals may be screened, but only in the context of a clinical research setting. Individuals who screen positive will be counseled about the risk of developing diabetes, diabetes symptoms, and the prevention of DKA. Numerous clinical studies are being conducted to test various methods of preventing type 1 diabetes in those with evidence of autoimmunity www. Screen for undiagnosed type 2 diabetes at the first prenatal visit in those with risk factors, using standard diagnostic criteria.
Screen for GDM at 24—28 weeks of gestation in pregnant women not previously known to have diabetes. Screen women with GDM for persistent diabetes at 6—12 weeks postpartum, using the OGTT and nonpregnancy diagnostic criteria. Women with a history of GDM should have lifelong screening for the development of diabetes or prediabetes at least every 3 years. Women with a history of GDM found to have prediabetes should receive lifestyle interventions or metformin to prevent diabetes.
Further research is needed to establish a uniform approach to diagnosing GDM. For many years, GDM was defined as any degree of glucose intolerance with onset or first recognition during pregnancy 13whether or not the condition persisted after pregnancy, and not excluding the possibility that unrecognized glucose intolerance may have antedated or begun concomitantly with the pregnancy.
This definition facilitated a uniform strategy for detection and classification of GDM, but its limitations were recognized for many years. As the ongoing epidemic of obesity and diabetes has led to more type 2 diabetes in women of childbearing age, the number of pregnant women with undiagnosed type 2 diabetes has increased Because of this, it is reasonable to screen women with risk factors for type 2 diabetes Table 4 at their initial prenatal visit, using standard diagnostic criteria Table 2.
Women with diabetes in the first trimester should receive a diagnosis of overt, not gestational, diabetes. GDM carries risks for the mother and neonate. Not all adverse outcomes are of equal clinical importance. For most complications, there was no threshold for risk.
These results have led to careful reconsideration of the diagnostic criteria for GDM. GDM screening can be accomplished with either of two strategies:. In the Standards of Care 44ADA for the first time recommended that all pregnant women not known to have prior diabetes undergo a g OGTT at 24—28 weeks of gestation based on an International Association of Diabetes and Pregnancy Study Groups IADPSG consensus meeting Diagnostic cut points for the fasting, 1-h, and 2-h PG measurements were defined that conveyed an odds ratio for adverse outcomes of at least 1.
The expected benefits to these pregnancies and offspring are inferred from intervention trials that focused on women with lower levels of hyperglycemia than identified using older GDM diagnostic criteria and that found modest benefits including reduced rates of large-for-gestational-age LGA births 46 However, while treatment of lower threshold hyperglycemia can reduce LGA, it has not been shown to reduce primary cesarean delivery rates.
Data are lacking on how treatment of lower threshold hyperglycemia impacts prognosis of future diabetes for the mother and future obesity, diabetes risk, or other metabolic consequences for the offspring. The frequency of follow-up and blood glucose monitoring for these women has also not yet been standardized, but is likely to be less intensive than for women diagnosed by the older criteria.
Moreover, screening with a g GLT does not require fasting and is therefore easier to accomplish for many women. Treatment of higher threshold maternal hyperglycemia, as identified by the two-step approach, reduces rates of neonatal macrosomia, LGA, and shoulder dystocia, without increasing small-for-gestational-age births How do two different groups of experts arrive at different GDM screening and diagnosis recommendations?
Because glycemic dysregulation exists on a continuum, the decision to pick a single binary threshold for diagnosis requires balancing the harms and benefits associated with greater versus lesser sensitivity.
Moreover, there are no available cost-effective analyses to examine the balance of achieved benefits versus the increased costs generated by this strategy. There are insufficient data to strongly demonstrate the superiority of one strategy over the other. The decision of which strategy to implement must therefore be made based on the relative values placed on currently unmeasured factors e. There remains strong consensus that establishing a uniform approach to diagnosing GDM will have extensive benefits for patients, caregivers, and policymakers.
Longer-term outcome studies are currently underway. Because some cases of GDM may represent preexisting undiagnosed type 2 diabetes, women with a history of GDM should be screened for diabetes 6—12 weeks postpartum, using nonpregnant OGTT criteria.
Because of their antepartum treatment for hyperglycemia, A1C for diagnosis of persistent diabetes at the postpartum visit is not recommended Women with a history of GDM have a greatly increased subsequent diabetes risk 51 and should be followed up with subsequent screening for the development of diabetes or prediabetes, as outlined in Section II.
Lifestyle interventions or metformin should be offered to women with a history of GDM who develop prediabetes, as discussed in Section IV. In the prospective Nurses' Health Study II, subsequent diabetes risk after a history of GDM was significantly lower in women who followed healthy eating patterns.
Adjusting for BMI moderately, but not completely, attenuated this association Patients with IGT AIFG Eor an A1C 5. Based on the cost-effectiveness of diabetes prevention, such programs should be covered by third-party payers. Metformin therapy for prevention of type 2 diabetes may be considered in those with IGT AIFG Eor an A1C 5.
At least annual monitoring for the development of diabetes in those with prediabetes is suggested. Screening for and treatment of modifiable risk factors for CVD is suggested.
RCTs have shown that individuals at high risk for developing type 2 diabetes IFG, IGT, or both can significantly decrease the rate of diabetes onset with particular interventions 23 — Diabetes Prevention Program Outcomes Study DPPOS A cost-effectiveness model suggested that lifestyle interventions as delivered in the DPP are cost-effective 56and actual cost data from the DPP and DPPOS confirm that lifestyle interventions are highly cost-effective Group delivery of the DPP intervention in community settings has the potential to be significantly less expensive while still achieving similar weight loss The Centers for Disease Control and Prevention CDC helps coordinate the National Diabetes Prevention Program, a resource designed to bring evidence-based lifestyle change programs for preventing type 2 diabetes to communities http: Given the clinical trial results and the known risks of progression of prediabetes to diabetes, persons with an A1C of 5.
Metformin has a strong evidence base and demonstrated long-term safety as pharmacological therapy for diabetes prevention For other drugs, cost, side effects, and lack of a persistent effect require consideration Metformin was less effective than lifestyle modification in the DPP and DPPOS, but may be cost-saving over a year period Metformin therefore might reasonably be recommended for very-high-risk individuals e.
People with prediabetes often have other cardiovascular risk factors, such as obesity, hypertension, and dyslipidemia, and are at increased risk for CVD events.
While treatment goals are the same as for other patients without diabetes, increased vigilance is warranted to identify and treat these and other risk factors e.
A complete medical evaluation should be performed to classify the diabetes, detect the presence of diabetes complications, review previous treatment and risk factor control in patients with established diabetes, assist in formulating a management plan, and provide a basis for continuing care.
A focus on the components of comprehensive care Table 7 will enable the health care team to optimally manage the patient with diabetes. In this collaborative and integrated team approach, the individuals with diabetes must also assume an active role in their care. The management plan should be formulated as a collaborative therapeutic alliance among the patient and family, the physician, and other members of the health care team.
A variety of strategies and techniques should be used to provide adequate education and development of problem-solving skills in the numerous aspects of diabetes management. Treatment goals and plans should be individualized and take patient preferences into account. The management plan should recognize diabetes self-management education DSME and ongoing diabetes support as integral components of care.
Two primary techniques are available for health providers and patients to assess the effectiveness of the management plan on glycemic control: Patients on multiple-dose insulin MDI or insulin pump therapy should do SMBG prior to meals and snacks, occasionally postprandially, at bedtime, prior to exercise, when they suspect low blood glucose, after treating low blood glucose until they are normoglycemic, and prior to critical tasks such as driving.
When prescribing SMBG, ensure that patients receive ongoing instruction and regular evaluation of SMBG technique and SMBG results, as well as their ability to use SMBG data to adjust therapy. Although the evidence for A1C lowering is less strong in children, teens, and younger adults, CGM may be helpful in these groups.
Success correlates with adherence to ongoing use of the device. Major clinical trials of insulin-treated patients that demonstrated the benefits of intensive glycemic control on diabetes complications have included SMBG as part of multifactorial interventions, suggesting that SMBG is a component of effective therapy. SMBG allows patients to evaluate their individual response to therapy and assess whether glycemic targets are being achieved.
Results of SMBG can be useful in preventing hypoglycemia and adjusting medications particularly prandial insulin dosesmedical nutrition therapy MNTand physical activity. Evidence also supports a correlation between SMBG frequency and lower A1C SMBG is especially important for patients treated with insulin to monitor for and prevent asymptomatic hypoglycemia and hyperglycemia.
Most patients with type 1 diabetes or on intensive insulin regimens MDI or insulin pump therapy should consider SMBG prior to meals and snacks, occasionally postprandially, at bedtime, prior to exercise, when they suspect low blood glucose, after treating low blood glucose until they are normoglycemic, and prior to critical tasks such as driving.
For many patients, this will require testing 6—8 times daily, although individual needs may vary. For patients on nonintensive insulin regimens, such as those with type 2 diabetes on basal insulin, when to prescribe SMBG and the testing frequency are unclear because there is insufficient evidence for testing in this cohort.
Several randomized trials have called into question the clinical utility and cost-effectiveness of routine SMBG in noninsulin-treated patients 64 — A recent meta-analysis suggested that SMBG reduced A1C by 0. A key consideration is that SMBG alone does not lower blood glucose level; to be useful, the information must be integrated into clinical and self-management plans.
Optimal use of SMBG requires proper review and interpretation of the data, both by the patient and provider. Among patients who checked their blood glucose at least once daily, many reported taking no action when results were high or low Patients should be taught how to use SMBG data to adjust food intake, exercise, or pharmacological therapy to achieve specific goals.
The ongoing need for and frequency of SMBG should be reevaluated at each routine visit. Real-time CGM through the measurement of interstitial glucose which correlates well with plasma glucose is available. These sensors require calibration with SMBG, and the latter are still required for making acute treatment decisions. CGM devices have alarms for hypo- and hyperglycemic excursions. The greatest predictor of A1C lowering for all age-groups was frequency of sensor use, which was lower in younger age-groups.
A CGM device equipped with an automatic low glucose suspend feature was recently approved by the U. Food and Drug Administration FDA.
The ASPIRE trial of patients showed that sensor-augmented insulin pump therapy with a low glucose suspend significantly reduced nocturnal hypoglycemia, without increasing A1C levels for those over 16 years of age These devices may offer the opportunity to reduce severe hypoglycemia for those with a history of nocturnal hypoglycemia.
However, before CGM is widely adopted, data must be reported and analyzed using a standard universal template that is predictable and intuitive Perform the A1C test at least two times a year in patients who are meeting treatment goals and who have stable glycemic control. Perform the A1C test quarterly in patients whose therapy has changed or who are not meeting glycemic goals. Use of POC testing for A1C provides the opportunity for more timely treatment changes.
A1C reflects average glycemia over several months 69 and has strong predictive value for diabetes complications 76 Thus, A1C testing should be performed routinely in all patients with diabetes: Some patients with stable glycemia well within target may do well with testing only twice per year. Unstable or highly intensively managed patients e. As mentioned above, the A1C test is subject to certain limitations. A1C also does not provide a measure of glycemic variability or hypoglycemia. For patients prone to glycemic variability, especially type 1 diabetic patients or type 2 diabetic patients with severe insulin deficiency, glycemic control is best evaluated by the combination of results from self-monitoring and the A1C.
The table in pre versions of the Standards of Medical Care in Diabetes describing the correlation between A1C and mean glucose was derived from relatively sparse data one 7-point profile over 1 day per A1C reading in the primarily non-Hispanic white type 1 diabetic participants in the DCCT Whether there are significant differences in how A1C relates to average glucose in children or in African American patients is an area for further study 33 For the time being, the question has not led to different recommendations about testing A1C or to different interpretations of the clinical meaning of given levels of A1C in those populations.
Other measures of chronic glycemia such as fructosamine are available, but their linkage to average glucose and their prognostic significance are not as clear as for A1C. Appropriate patients might include those with short duration of diabetes, long life expectancy, and no significant CVD. Hyperglycemia defines diabetes, and glycemic control is fundamental to diabetes management. The DCCT study 76a prospective RCT of intensive versus standard glycemic control in patients with relatively recently diagnosed type 1 diabetes showed definitively that improved glycemic control is associated with significantly decreased rates of microvascular retinopathy and nephropathy and neuropathic complications.
Follow-up of the DCCT cohorts in the Epidemiology of Diabetes Interventions and Complications EDIC study 8283 demonstrated persistence of these microvascular benefits in previously intensively treated subjects, even though their glycemic control approximated that of previous standard arm subjects during follow-up.
The Kumamoto 84 and UK Prospective Diabetes Study UKPDS 8586 confirmed that intensive glycemic control was associated with significantly decreased rates of microvascular and neuropathic complications in type 2 diabetic patients.
Long-term follow-up of the UKPDS cohorts showed enduring effects of early glycemic control on most microvascular complications Three landmark trials ACCORD, ADVANCE, and VADT, described in further detail below were designed to examine the impact of intensive A1C control on CVD outcomes and showed that lower A1C levels were associated with reduced onset or progression of microvascular complications 88 — Epidemiological analyses of the DCCT and UKPDS 7677 demonstrate a curvilinear relationship between A1C and microvascular complications.
Given the substantially increased risk of hypoglycemia in type 1 diabetes trials, and now seen in recent type 2 diabetes trials, the risks of lower glycemic targets may outweigh the potential benefits on microvascular complications on a population level. The concerning mortality findings in the ACCORD trial 91 and the relatively much greater effort required to achieve near-euglycemia should also be considered when setting glycemic targets. However, based on physician judgment and patient preferences, select patients, especially those with little comorbidity and long life expectancy, may benefit from adopting more intensive glycemic targets e.
CVD is a more common cause of death than microvascular complications in populations with diabetes. However, it is less clearly impacted by hyperglycemia levels or intensity of glycemic control. In the DCCT, there was a trend toward lower risk of CVD events with intensive control.
The benefit of intensive glycemic control in this type 1 diabetic cohort has recently been shown to persist for several decades In type 2 diabetes, there is evidence that more intensive treatment of glycemia in newly diagnosed patients may reduce long-term CVD rates.
The Action to Control Cardiovascular Risk in Diabetes ACCORDAction in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation ADVANCEand the Veterans Affairs Diabetes Trial VADT studies suggested no significant reduction in CVD outcomes with intensive glycemic control in participants who had more advanced type 2 diabetes than UKPDS participants.
All three trials were conducted in participants with more long-standing diabetes mean duration 8—11 years and either known CVD or multiple cardiovascular risk factors. Details of these studies are reviewed extensively in an ADA position statement The glycemic control comparison was halted early due to an increased mortality rate in the intensive compared with the standard arm 1. Initial analysis of the ACCORD data evaluating variables including weight gain, use of any specific drug or drug combination, and hypoglycemia did not identify a clear explanation for the excess mortality in the intensive arm There was no A1C level at which intensive versus standard arm participants had significantly lower mortality.
The highest risk for mortality was observed in intensive arm participants with the highest A1C levels Severe hypoglycemia was significantly more likely in participants randomized to the intensive glycemic control arm.
The primary outcome of ADVANCE was a combination of microvascular events nephropathy and retinopathy and major adverse cardiovascular events MI, stroke, and cardiovascular death. There was no difference in overall or cardiovascular mortality between the two arms The primary outcome of the VADT was a composite of CVD events.
The trial randomized type 2 diabetic participants who were uncontrolled on insulin or on maximal dose oral agents median entry A1C 9. The cumulative primary outcome was nonsignificantly lower in the intensive arm An ancillary study of the VADT demonstrated that intensive glycemic control significantly reduced the primary CVD outcome in individuals with less atherosclerosis at baseline but not in persons with more extensive baseline atherosclerosis A post hoc analysis showed that mortality in the intensive versus standard glycemic control arm was related to duration of diabetes at study enrollment.
Those with diabetes duration less than 15 years had a mortality benefit in the intensive arm, while those with duration of 20 years or more had higher mortality in the intensive arm The evidence for a cardiovascular benefit of intensive glycemic control primarily rests on long-term follow-up of study cohorts treated early in the course of type 1 and type 2 diabetes, and a subset analyses of ACCORD, ADVANCE, and VADT.
However, heterogeneity of the mortality effects across studies was noted. A prespecified subgroup analysis suggested that major CVD outcome reduction occurred in patients without known CVD at baseline HR 0.
Conversely, the mortality findings in ACCORD and subgroup analyses of the VADT suggest that the potential risks of intensive glycemic control may outweigh its benefits in some patients. Providers should be vigilant in preventing severe hypoglycemia in patients with advanced disease and should not aggressively attempt to achieve near-normal A1C levels in patients in whom such targets cannot be safely and reasonably achieved. Severe or frequent hypoglycemia is an absolute indication for the modification of treatment regimens, including setting higher glycemic goals.
Approach to management of hyperglycemia. Depiction of the elements of decision making used to determine appropriate efforts to achieve glycemic targets. Where possible, such decisions should be made in conjunction with the patient, reflecting his or her preferences, needs, and values.
Adapted with permission from Ismail-Beigi et al. Recommended glycemic goals for many nonpregnant adults are shown in Table 9. The issue of pre- versus postprandial SMBG targets is complex Elevated postchallenge 2-h OGTT glucose values have been associated with increased cardiovascular risk independent of FPG in some epidemiological studies. In diabetic subjects, surrogate measures of vascular pathology, such as endothelial dysfunction, are negatively affected by postprandial hyperglycemia However, outcome studies have clearly shown A1C to be the primary predictor of complications, and landmark glycemic control trials such as the DCCT and UKPDS relied overwhelmingly on preprandial SMBG.
Additionally, an RCT in patients with known CVD found no CVD benefit of insulin regimens targeting postprandial glucose compared with those targeting preprandial glucose Summary of glycemic recommendations for many nonpregnant adults with diabetes. The goals for glycemic control for women with GDM are based on recommendations from the Fifth International Workshop-Conference on Gestational Diabetes Mellitus and have the following targets for maternal capillary glucose concentrations:.
For women with preexisting type 1 or type 2 diabetes who become pregnant, the following are recommended as optimal glycemic goals, if they can be achieved without excessive hypoglycemia Most people with type 1 diabetes should be treated with MDI injections three to four injections per day of basal and prandial insulin or continuous subcutaneous insulin infusion CSII.
Most people with type 1 diabetes should be educated in how to match prandial insulin dose to carbohydrate intake, premeal blood glucose, and anticipated activity. Most people with type 1 diabetes should use insulin analogs to reduce hypoglycemia risk.
Consider screening those with type 1 diabetes for other autoimmune diseases thyroid, vitamin B 12 deficiency, celiac as appropriate. The DCCT clearly showed that intensive insulin therapy three or more injections per day of insulin, or CSII or insulin pump therapy was a key part of improved glycemia and better outcomes 76 The study was carried out with short- and intermediate-acting human insulins. Despite better microvascular outcomes, intensive insulin therapy was associated with a high rate of severe hypoglycemia 62 episodes per patient-years of therapy.
Since the DCCT, a number of rapid-acting and long-acting insulin analogs have been developed. These analogs are associated with less hypoglycemia with equal A1C lowering in type 1 diabetes Use MDI injections 3—4 injections per day of basal and prandial insulin or CSII therapy.
Match prandial insulin to carbohydrate intake, premeal blood glucose, and anticipated activity. There are excellent reviews to guide the initiation and management of insulin therapy to achieve desired glycemic goals, Although most studies of MDI versus pump therapy have been small and of short duration, a systematic review and meta-analysis concluded that there were no systematic differences in A1C or severe hypoglycemia rates in children and adults between the two forms of intensive insulin therapy Recently, a large randomized trial in type 1 diabetic patients with nocturnal hypoglycemia reported that sensor-augmented insulin pump therapy with the threshold-suspend feature reduced nocturnal hypoglycemia, without increasing glycated hemoglobin values For selected individuals who have mastered carbohydrate counting, education on the impact of protein and fat on glycemic excursions can be incorporated into diabetes management Because of the increased frequency of other autoimmune diseases in type 1 diabetes, screening for thyroid dysfunction, vitamin B 12 deficiency, and celiac disease should be considered based on signs and symptoms.
Periodic screening in asymptomatic individuals has been recommended, but the effectiveness and optimal frequency are unclear.
Metformin, if not contraindicated and if tolerated, is the preferred initial pharmacological agent for type 2 diabetes. If noninsulin monotherapy at maximum tolerated dose does not achieve or maintain the A1C target over 3 months, add a second oral agent, a glucagon-like peptide 1 GLP-1 receptor agonist, or insulin.
A patient-centered approach should be used to guide choice of pharmacological agents. Considerations include efficacy, cost, potential side effects, effects on weight, comorbidities, hypoglycemia risk, and patient preferences.
Due to the progressive nature of type 2 diabetes, insulin therapy is eventually indicated for many patients with type 2 diabetes. The ADA and the European Association for the Study of Diabetes EASD formed a joint task force to evaluate the data and develop recommendations for the use of antihyperglycemic agents in type 2 diabetic patients This position statement is less prescriptive than prior algorithms and discusses advantages and disadvantages of the available medication classes and considerations for their use.
A patient-centered approach is stressed, including patient preferences, cost and potential side effects of each class, effects on body weight, and hypoglycemia risk.
The position statement reaffirms metformin as the preferred initial agent, barring contraindication or intolerance, either in addition to lifestyle counseling and support for weight loss and exercise, or when lifestyle efforts alone have not achieved or maintained glycemic goals. Metformin has a long-standing evidence base for efficacy and safety, is inexpensive, and may reduce risk of cardiovascular events When metformin fails to achieve or maintain glycemic goals, another agent should be added.
Although there are numerous trials comparing dual therapy to metformin alone, few directly compare drugs as add-on therapy. Comparative effectiveness meta-analyses suggest that overall, each new class of noninsulin agents added to initial therapy lowers A1C around 0.
Many patients with type 2 diabetes eventually require and benefit from insulin therapy. The progressive nature of type 2 diabetes and its therapies should be regularly and objectively explained to patients. Providers should avoid using insulin as a threat or describing it as a failure or punishment. Equipping patients with an algorithm for self-titration of insulin doses based on SMBG results improves glycemic control in type 2 diabetic patients initiating insulin Refer to the ADA-EASD position statement for more details on pharmacotherapy for hyperglycemia in type 2 diabetes Fig.
Antihyperglycemic therapy in type 2 diabetes: DPPi, DPP-4 inhibitor; Fx's, bone fractures; GI, gastrointestinal; GLPRA, GLP-1 receptor agonist; HF, heart failure; SU, sulfonylurea; TZD, thiazolidinedione. For further details, see ref. Nutrition therapy is recommended for all people with type 1 and type 2 diabetes as an effective component of the overall treatment plan.
Individuals who have prediabetes or diabetes should receive individualized MNT as needed to achieve treatment goals, preferably provided by a registered dietitian familiar with the components of diabetes MNT. Because diabetes nutrition therapy can result in cost savings B and improved outcomes such as reduction in A1C Anutrition therapy should be adequately reimbursed by insurance and other payers.
For overweight or obese adults with type 2 diabetes or at risk for diabetes, reducing energy intake while maintaining a healthful eating pattern is recommended to promote weight loss. To achieve modest weight loss, intensive lifestyle interventions counseling about nutrition therapy, physical activity, and behavior change with ongoing support are recommended. Evidence suggests that there is not an ideal percentage of calories from carbohydrate, protein, and fat for all people with diabetes B ; therefore, macronutrient distribution should be based on individualized assessment of current eating patterns, preferences, and metabolic goals.
A variety of eating patterns combinations of different foods or food groups are acceptable for the management of diabetes. Monitoring carbohydrate intake, whether by carbohydrate counting or experience-based estimation, remains a key strategy in achieving glycemic control. For good health, carbohydrate intake from vegetables, fruits, whole grains, legumes, and dairy products should be advised over intake from other carbohydrate sources, especially those that contain added fats, sugars, or sodium.
Substituting low-glycemic load foods for higher-glycemic load foods may modestly improve glycemic control. People with diabetes should consume at least the amount of fiber and whole grains recommended for the general public. While substituting sucrose-containing foods for isocaloric amounts of other carbohydrates may have similar blood glucose effects, consumption should be minimized to avoid displacing nutrient-dense food choices. People with diabetes and those at risk for diabetes should limit or avoid intake of sugar-sweetened beverages from any caloric sweetener including high-fructose corn syrup and sucrose to reduce risk for weight gain and worsening of cardiometabolic risk profile.
Evidence is inconclusive for an ideal amount of total fat intake for people with diabetes; therefore, goals should be individualized. C Fat quality appears to be far more important than quantity. In people with type 2 diabetes, a Mediterranean-style, MUFA-rich eating pattern may benefit glycemic control and CVD risk factors and can therefore be recommended as an effective alternative to a lower-fat, higher-carbohydrate eating pattern.
As recommended for the general public, an increase in foods containing long-chain n-3 fatty acids EPA and DHA from fatty fish and n-3 linolenic acid ALA is recommended for individuals with diabetes because of their beneficial effects on lipoproteins, prevention of heart disease, and associations with positive health outcomes in observational studies. The amount of dietary saturated fat, cholesterol, and trans fat recommended for people with diabetes is the same as that recommended for the general population.
There is no clear evidence of benefit from vitamin or mineral supplementation in people with diabetes who do not have underlying deficiencies. Routine supplementation with antioxidants, such as vitamins E and C and carotene, is not advised because of lack of evidence of efficacy and concern related to long-term safety.
Evidence does not support recommending n-3 EPA and DHA supplements for people with diabetes for the prevention or treatment of cardiovascular events. There is insufficient evidence to support the routine use of micronutrients such as chromium, magnesium, and vitamin D to improve glycemic control in people with diabetes.
If adults with diabetes choose to drink alcohol, they should be advised to do so in moderation one drink per day or less for adult women and two drinks per day or less for adult men.
Alcohol consumption may place people with diabetes at increased risk for delayed hypoglycemia, especially if taking insulin or insulin secretagogues. Education and awareness regarding the recognition and management of delayed hypoglycemia is warranted. For individuals with both diabetes and hypertension, further reduction in sodium intake should be individualized. Individuals at high risk for type 2 diabetes should be encouraged to achieve the U.
The ADA recently released an updated position statement on nutrition therapy for adults living with diabetes Nutrition therapy is an integral component of diabetes prevention, management, and self-management education. All individuals with diabetes should receive individualized MNT preferably provided by a registered dietitian who is knowledgeable and skilled in providing diabetes MNT.
Comprehensive group diabetes education programs including nutrition therapy or individualized education sessions have reported A1C decreases of 0. Individuals with type 1 diabetes should be offered intensive insulin therapy education using the carbohydrate-counting meal planning approach, — ; this approach has been shown to improve glycemic control Consistent carbohydrate intake with respect to time and amount can result in improved glycemic control for individuals using fixed daily insulin doses A simple diabetes meal planning approach such as portion control or healthful food choices may be better suited for individuals with health literacy and numeracy concerns — Weight loss of 2—8 kg may provide clinical benefits in those with type 2 diabetes, especially early in the disease process — Weight loss studies have used a variety of energy-restricted eating patterns, with no clear evidence that one eating pattern or optimal macronutrient distribution was ideal.
Although several studies resulted in improvements in A1C at 1 year, —not all weight loss interventions led to 1-year A1C improvements— The most consistently can you really earn money by taking online surveys changes in cardiovascular risk factors were an increase in HDL cholesterol,, decrease in triglycerides, and decrease in blood pressure, Intensive lifestyle programs with frequent follow-up are required to achieve significant reductions in excess body weight and improve clinical indicators Several studies have attempted to identify the optimal mix of macronutrients for meal plans of people with diabetes.
However, a recent systematic review found that there was no ideal macronutrient distribution and that macronutrient proportions should be individualized. A variety of eating patterns have been shown to be effective in managing diabetes, including Mediterranean-style,Dietary Approaches to Stop Hypertension DASH -styleplant-based vegan or vegetarianlower-fatand lower-carbohydrate patterns Studies examining the ideal amount is it a good idea to buy stock before it splits carbohydrate intake for people with diabetes are inconclusive, although monitoring carbohydrate intake and considering the available insulin are key strategies for improving postprandial glucose control, In many studies, it is often difficult to discern the independent effect of fiber compared with that of glycemic index on glycemic control and other outcomes.
Improvements in CVD risk measures are overseas stock broker Recent studies have shown modest effect of fiber on lowering preprandial glucose and mixed results on improving CVD risk factors. A systematic review found consumption of forex jitu grains earnest money edina realty not associated with improvements in glycemic control in people with type 2 diabetes, although it may reduce systemic inflammation.
One study did find a potential benefit of whole grain intake in reducing mortality and CVD Limited research exists concerning the ideal amount of fat for individuals with diabetes.
This AMDR was based on evidence for CHD risk with a low intake of fat and high intake of carbohydrate, and evidence for increased obesity and CHD with high intake of fat The type of fatty acids consumed is more important than total amount of fat when looking at metabolic goals and risk of CVD, Some of these studies also included caloric restriction, which may have contributed to improvements in glycemic control or blood lipids The ideal ratio of n-6 to n-3 fatty acids has not been determined; however, PUFA and MUFA are recommended substitutes for saturated or trans fat A recent systematic review concluded that supplementation with n-3 fatty acids did not improve glycemic control but that higher dose supplementation decreased triglycerides in individuals with type 2 diabetes.
Diabetes Care
Three longer-duration studies also reported mixed outcomes — Thus, RCTs do not clearing forex bank recommending n-3 supplements for primary or secondary prevention of CVD. Little evidence has been published about the relationship between dietary intake of saturated fatty acids and dietary cholesterol and glycemic control and CVD risk in people with diabetes.
Therefore, people with diabetes eur usd exchange rate april 2012 follow the guidelines for the general population for the recommended intakes of saturated fat, dietary cholesterol, and trans fat Published data on the effects of plant stanols and sterols on CVD risk in individuals with diabetes include four RCTs that reported beneficial effects for total, Capital option binary trading, and non-HDL cholesterol — There is limited evidence that the use of vitamin, mineral, or herbal supplements is necessary in the management of diabetes — Limited studies have been published on sodium reduction in people with diabetes.

A recent Cochrane review found that decreasing sodium intake reduces blood pressure in those with diabetes However, two other studies in type 1 diabetes and kurs walut onet forex 2 diabetes have warranted caution for universal sodium restriction to 1, mg in this population.
Goal sodium intake recommendations should take into account palatability, availability, additional cost of specialty low sodium products, and the difficulty of achieving both low sodium recommendations and a nutritionally adequate diet People with diabetes should receive DSME and diabetes self-management support DSMS according to National Standards for Diabetes Self-Management Education and Support when their diabetes is diagnosed and as needed thereafter.
Effective self-management and quality of life are the key outcomes of DSME and DSMS and should be measured and monitored as part of care. DSME and DSMS should address psychosocial issues, since emotional well-being is associated with positive diabetes outcomes. DSME and DSMS programs are appropriate venues for people with prediabetes to receive education and support to develop and maintain behaviors that can prevent or delay the onset of diabetes.
Because DSME and DSMS can result in cost-savings and improved outcomes BDSME and Pardo evaluation and optimization of trading strategies should be adequately reimbursed by third-party payers.
DSME and DSMS are the ongoing processes of facilitating the knowledge, skill, and ability necessary for diabetes self-care. This process incorporates the needs, goals, and life experiences of the person with diabetes. The overall objectives of DSME and DSMS are to support informed decision making, self-care behaviors, problem solving, and active collaboration with the health care team to improve clinical outcomes, health status, and quality of life in a cost-effective manner DSME and DSMS are essential elements of diabetes care —and the current National Standards for Diabetes Self-Management Education and Support are based on evidence for their benefits.
Education helps people with diabetes initiate effective self-management and cope with diabetes when they are first diagnosed. Ongoing DSME and DSMS also help people with diabetes maintain effective self-management throughout a lifetime of diabetes as they face new challenges and treatment advances become available. DSME enables patients including youth to optimize metabolic control, prevent and manage complications, and maximize quality of life, in a cost-effective manner Current best practice of DSME is a skills-based approach that focuses on helping those with diabetes make informed self-management choices DSME has changed from a didactic approach focusing on providing information to more theoretically based empowerment models that focus on helping those with diabetes make informed self-management decisions Diabetes care has shifted to an approach that is more patient centered and places the person with diabetes and his or her family at the center of the care model working in collaboration with health care professionals.
Patient-centered care is respectful of and responsive to individual patient preferences, needs, and values and ensures that patient values guide all decision making Multiple studies have found that DSME is associated with improved diabetes knowledge and improved self-care behavior, improved clinical outcomes such as lower Forex ghl indicator—lower self-reported weightimproved quality of life,healthy coping, and lower costs Better outcomes were reported for DSME interventions that were longer trans livestock trading included follow-up support DSMS—that were culturallyand age appropriateand were tailored to individual needs and preferences, and that addressed psychosocial issues and incorporated behavioral strategies, — Both individual and group approaches have been found effective Diabetes education is associated with increased use of primary and preventive services, and lower use of acute, inpatient hospital services Patients who participate in diabetes education are more likely to follow best practice treatment recommendations, particularly among the Medicare population, and have lower Medicare and commercial claim costs The National Standards for Diabetes Self-Management Education and Support are designed to define quality DSME and DSMS and to assist diabetes educators in a variety of settings to provide evidence-based education and self-management support The standards are reviewed and updated every 5 years by a task force representing key gts global trading systems involved in the field of diabetes education and care.
The standards for DSME and DSMS also apply to the education and support of people with prediabetes. Currently, there are significant barriers to the provision of education and support to those with prediabetes. However, the strategies for supporting successful behavior change and the healthy behaviors recommended for people with prediabetes are largely identical to those for people with diabetes. As barriers to care are overcome, providers of DSME and DSMS, given their training and experience, are particularly well equipped to assist people with prediabetes in developing and maintaining behaviors that can prevent or delay the onset of diabetes, DSME, when provided by a program that meets national standards for DSME and is recognized by ADA forex brokers in ontario other approval bodies, is reimbursed as part of the Medicare program as overseen by the Centers for Medicare and Medicaid Services CMS.
DSME is also covered by most health insurance plans. As is the case for all children, children with diabetes or prediabetes should be action forex heat map to engage in at least 60 min of physical activity each day. In productive strategy in binary options 60 sec absence of contraindications, adults with type 2 diabetes should be encouraged to perform resistance training at least twice per week.
Exercise is an important part of the diabetes management plan. Lyrics to the song money maker by too short exercise has been shown to improve blood glucose control, reduce cardiovascular risk factors, contribute to weight loss, and improve well-being.
Furthermore, regular exercise may prevent type 2 diabetes in high-risk profiting in forex 23 — There are considerable data for the health benefits e.
Higher levels of exercise intensity are associated with greater improvements in A1C and in fitness Other benefits include slowing the decline in mobility among overweight patients with diabetes A joint position statement of ADA and the American College of Sports Medicine summarizes the evidence for how confident to trade the binary options profitably review benefits of exercise in people with type 2 diabetes The guidelines suggest that adults over age 65 years, or those with disabilities, follow the adult guidelines if possible or if this is not possible be as physically active as they are able.
Studies included in the meta-analysis of effects of exercise interventions on glycemic control had a mean of 3. Therefore, it seems reasonable to recommend that people with diabetes follow the physical activity guidelines for the general population. Progressive resistance exercise improves insulin sensitivity in older men with type 2 diabetes to the same or even a greater extent as aerobic exercise Clinical trials have provided strong evidence for the A1C lowering value of resistance training in older adults with type 2 diabetes, and for an additive benefit of combined aerobic and resistance exercise in adults with type 2 diabetes In the absence of contraindications, ato tax share trader with type 2 diabetes should be encouraged to do at least two weekly sessions of resistance exercise exercise with free weights or weight machineswith each session consisting of at least one set of five or more different resistance exercises involving the large muscle groups As discussed more how much money does the blues clues guy make in Section VI.
An ADA consensus statement on this issue concluded that routine screening is not recommended Providers should use clinical judgment in this area.
Certainly, high-risk patients should be encouraged to start with short periods of low-intensity exercise and increase the intensity and duration slowly. Providers should assess patients for conditions that might contraindicate certain types of exercise or predispose to injury, such as uncontrolled hypertension, severe autonomic neuropathy, severe peripheral neuropathy or history of foot lesions, and unstable proliferative retinopathy.
Those with complications may require a more thorough evaluation When people with type 1 diabetes are deprived of insulin for 12—48 h and are ketotic, exercise can worsen hyperglycemia and ketosis ; therefore, vigorous activity should be avoided in the presence of ketosis.
Hypoglycemia is less common in diabetic individuals who are not treated with insulin or insulin secretagogues, and no preventive measures for hypoglycemia are usually advised in these cases. In the presence of proliferative diabetic retinopathy PDR or severe non-PDR NPDRvigorous aerobic or resistance exercise may be contraindicated because of the risk of triggering vitreous hemorrhage or retinal detachment Decreased pain sensation and a higher pain threshold in the extremities result in increased risk of skin breakdown and infection and of Charcot joint destruction with some forms of exercise.
However, studies have shown that moderate-intensity walking may not lead to increased risk of foot ulcers or reulceration in those with peripheral neuropathy All individuals with peripheral neuropathy should wear proper footwear and examine their feet daily to detect lesions early. Anyone with a foot injury or open sore should be restricted to non—weight-bearing activities.
Autonomic neuropathy can increase the risk of exercise-induced injury or adverse event through decreased cardiac responsiveness to exercise, postural hypotension, impaired thermoregulation, impaired night vision due to impaired papillary reaction, and higher susceptibility to hypoglycemia Cardiovascular autonomic neuropathy CAN is also an independent risk factor for cardiovascular death and silent myocardial ischemia Therefore, individuals with diabetic autonomic neuropathy should undergo cardiac investigation before beginning physical activity more intense than that to which they are accustomed.
Physical activity can acutely increase urinary protein excretion. However, there is no evidence that vigorous exercise increases the rate of progression of diabetic kidney disease and likely no need for any specific exercise restrictions for people with diabetic kidney disease Routinely screen for psychosocial problems such as depression and diabetes-related distress, anxiety, eating disorders, and cognitive impairment.
Emotional well-being is an important part of diabetes care and self-management. There are opportunities for the clinician to routinely assess psychosocial status in a timely and efficient manner so that referral for appropriate services can be accomplished. However, there was a limited association between the effects on A1C and mental health, and no intervention characteristics predicted benefit on both outcomes Key opportunities for routine screening of psychosocial status occur at diagnosis, during regularly scheduled management visits, during hospitalizations, with the discovery of complications, or when problems with glucose control, quality of life, or self-management are identified.
Patients are likely to exhibit psychological vulnerability at diagnosis and when their medical status changes, e. There appears to be a bidirectional relationship with both diabetes and metabolic syndrome and depression. Diabetes-related distress is distinct from clinical depression and is very common — among people with diabetes and their family members High levels of distress are significantly linked to A1C, self-efficacy, dietary and exercise behaviors, and medication taking Other issues known to impact self-management and health outcomes include but are not limited to attitudes about the illness, expectations for medical management and outcomes, anxiety, general and diabetes-related quality of life, resources financial, social, and emotional and psychiatric history Screening tools are available for a number of these areasmossberg 930 spx stock shims, Indications for referral to a mental health specialist familiar with diabetes management may include gross disregard for the medical regimen by self or othersdepression, possibility of self-harm, debilitating anxiety alone or with depressionindications of an eating disorderor cognitive functioning that significantly impairs judgment.
It is preferable to incorporate psychological assessment and treatment into routine care rather than waiting for a specific problem or deterioration in metabolic or psychological status In the recent DAWN2 study, significant diabetes-related distress was reported by Although the clinician may not feel qualified to treat psychological problemsusing the patient-provider relationship as a foundation can increase how to get unlimited money on the app store with cydia likelihood that the patient will accept referral for other services.
Collaborative care interventions and use of a team approach have demonstrated efficacy in diabetes and depression, and interventions to enhance self-management and address severe distress have demonstrated efficacy in diabetes-related distress Some people with diabetes and their health care providers may not achieve the desired treatment goals Table 9.
Rethinking the treatment regimen may require assessment of barriers including income, health literacy, diabetes-related distress, depression, and competing demands, including those related to family responsibilities and dynamics.
Other strategies may include culturally appropriate and enhanced DSME and DSMS, comanagement with a diabetes team, referral to a medical social worker for assistance with insurance coverage, assessing medication-taking behaviors, or change in pharmacological therapy. Initiation of or increase in SMBG, use of CGM, frequent contact with the patient, or referral to a mental health professional or physician with special expertise in diabetes may be useful.
Any condition leading to deterioration in glycemic control necessitates more frequent monitoring of blood glucose and in ketosis-prone patients urine or blood ketones. If accompanied by ketosis, vomiting, or alteration in level of consciousness, marked hyperglycemia requires temporary adjustment of the treatment regimen and immediate interaction with the diabetes care team. The patient treated with noninsulin therapies or MNT alone may temporarily require insulin. Adequate fluid and caloric intake must be assured.
Infection or dehydration is more likely to necessitate hospitalization of the person with diabetes than the person without diabetes. The hospitalized patient should be treated by a physician with expertise in diabetes management.
For further information on eclipse trading system of patients with hyperglycemia in the hospital, see Section IX. For further information on management of DKA or hyperglycemic nonketotic hyperosmolar state, earn money on your gap year to how to make money soccer trading ADA fx180 currency trading strategy on hyperglycemic crises Individuals at risk for hypoglycemia should be asked about symptomatic and asymptomatic hypoglycemia at each encounter.
Glucose 15—20 g is the preferred treatment for the conscious individual with hypoglycemia, although any form of carbohydrate that contains glucose may be used. After 15 min of treatment, if SMBG fidelity cost to buy stock continued hypoglycemia, the treatment should be repeated.
Once SMBG returns to normal, the individual should consume a meal or snack to prevent recurrence of hypoglycemia. Glucagon should be prescribed for all individuals at significant risk of severe hypoglycemia, and caregivers or family members of these individuals should be instructed on its administration.
Glucagon administration is not limited to health care professionals. Hypoglycemia unawareness or one or more episodes of severe hypoglycemia should trigger re-evaluation of the treatment regimen. Insulin-treated patients with hypoglycemia unawareness or an episode of severe hypoglycemia should be advised to raise their glycemic targets to strictly avoid further hypoglycemia for at least several weeks, to partially reverse hypoglycemia unawareness and reduce risk of future episodes.
Hypoglycemia is the leading limiting factor in the glycemic management of type 1 and insulin-treated type 2 diabetes Mild hypoglycemia may be inconvenient or frightening to patients with diabetes. Severe hypoglycemia can cause acute harm to the person with diabetes or others, especially if it causes falls, motor vehicle accidents, or other injury.
A large cohort study suggested that among older adults with type 2 diabetes, a stock market for beginners philippines of severe hypoglycemia was associated with greater risk of dementia Conversely, in a substudy of the ACCORD trial, cognitive impairment at baseline or decline in cognitive function during the trial was significantly associated with subsequent episodes of severe hypoglycemia As described in Section V.
An association of severe hypoglycemia with mortality was also found in the ADVANCE trial An association of self-reported severe hypoglycemia with 5-year mortality has also been reported in clinical practice InADA and The Endocrine Society published a consensus report on the impact and treatment of hypoglycemia on diabetic patients.
Severe hypoglycemia was defined as an event requiring assistance of another person. Young children with type 1 diabetes and the elderly were noted as particularly vulnerable due to their limited ability to recognize hypoglycemic symptoms and effectively communicate their needs. The report recommended that short-acting insulin sliding scales, often used in long-term care facilities, should be avoided and complex regimens simplified.
Individualized patient education, dietary intervention e. Hypoglycemia treatment requires ingestion of glucose- or carbohydrate-containing foods. The acute glycemic response correlates better with the glucose content than with the carbohydrate easy money maker club penguin online no download free of the food.
Pure glucose is the preferred treatment, but any form of carbohydrate that contains glucose will raise blood glucose. Added fat may retard and then prolong the acute glycemic response. Ongoing insulin activity or insulin secretagogues may lead to recurrent hypoglycemia unless further food is ingested after recovery. Those in close contact with, or having custodial care of, people with hypoglycemia-prone diabetes family members, roommates, school personnel, child care providers, correctional institution staff, or coworkers should be instructed on use of glucagon kits.
An individual does not need to be a health care professional to safely administer glucagon. A glucagon kit requires a prescription. Care should be taken to ensure that glucagon kits are not expired.
Hypoglycemia prevention is a critical component of diabetes management. SMBG and, for some patients, CGM are key tools to assess therapy and detect incipient hypoglycemia.
Patients should understand situations that increase their risk of hypoglycemia, such as when binary options long term strategy for tests or procedures, during or after intense exercise, and during sleep, and that hypoglycemia may increase the risk of harm to self or others, such as with driving.
Teaching people with diabetes to balance insulin use, carbohydrate intake, and exercise is a necessary but not always sufficient strategy for prevention.
In type 1 diabetes and severely insulin-deficient type 2 diabetes, hypoglycemia unawareness, or hypoglycemia-associated autonomic failure, can severely compromise stringent diabetes control and quality of life. The deficient counter-regulatory hormone release and autonomic responses in this syndrome are both risk factors for, and caused by, hypoglycemia.
Hence, patients with one or more episodes of severe hypoglycemia may benefit from at least short-term relaxation of glycemic targets. Patients with type 2 diabetes who have undergone bariatric surgery need lifelong lifestyle support and medical monitoring.
The long-term benefits, cost-effectiveness, and risks of bariatric surgery in individuals with type 2 diabetes should be studied in well-designed controlled trials with optimal medical and lifestyle therapy as the comparator. Remission rates tend to be lower with procedures that only constrict the stomach and higher with those that bypass portions of the small intestine. Additionally, intestinal bypass procedures may have glycemic effects that are independent of their effects on weight, perhaps involving the incretin axis.
There is also evidence for diabetes remission following bariatric surgery in persons with type 2 diabetes who are less severely obese. The latter group lost only 1. Bariatric surgery is costly in the short term and has associated risks. Morbidity and mortality rates directly related london forex market close time the surgery have been reduced considerably in recent years, with day mortality rates now 0.
Longer-term concerns include vitamin and mineral deficiencies, osteoporosis, and rare but often severe hypoglycemia from insulin hypersecretion. Cohort studies attempting to match subjects suggest that the procedure may reduce longer-term mortality rates Retrospective analyses and modeling studies suggest that these procedures may be cost-effective for patients with type 2 diabetes, when one considers reduction in subsequent health care costs— Caution about the benefits of bariatric surgery is warranted.
A propensity score-adjusted analyses of older severely obese patients with high baseline mortality in Veterans Affairs Medical Centers found that bariatric surgery was not associated with decreased mortality compared with usual care mean follow-up 6. Nearly one out of three patients experienced band erosion, and almost half had required removal of their bands.
Understanding the mechanisms of glycemic improvement, long-term benefits, and risks of bariatric surgery in individuals with type 2 diabetes, especially those who are not severely obese, will require well designed clinical trials, with optimal medical and lifestyle therapy, and cardiovascular risk factors as the comparator. Other indications for repeat vaccination include nephrotic syndrome, chronic renal disease, and other immunocompromised states, such as after transplantation.
Administer hepatitis B vaccination to unvaccinated adults with diabetes who are aged 19—59 years. Influenza and pneumonia are common, preventable infectious diseases associated with high mortality and morbidity in the elderly and in people with chronic diseases.
Though there are limited studies reporting the morbidity and mortality of influenza and pneumococcal pneumonia specifically in people with diabetes, observational studies of patients with a variety of chronic illnesses, including diabetes, show that these conditions are associated with an increase in hospitalizations analysis of binary options on sp500 futures 01112016 influenza and its complications.
Safe and effective vaccines that greatly reduce the risk of serious complications from these diseases are available There is sufficient evidence to support that people with diabetes have appropriate serologic and clinical responses to these vaccinations. The CDC Advisory Committee on Immunization Practices recommends influenza and pneumococcal vaccines for all individuals with diabetes http: Late inthe Advisory Committee on Immunization Practices of the CDC recommended that all previously unvaccinated adults with diabetes aged 19—59 years be vaccinated against hepatitis B virus HBV as soon as possible after a diagnosis of diabetes is made.
Additionally, after assessing risk and likelihood of an adequate immune response, vaccinations for those aged 60 years and over should also be considered HBV is highly transmissible and stable for long periods of time on surfaces such as lancing wow gold making professions mop and blood glucose meters, even when no blood is visible.
Blood sufficient to transmit the virus has also been found in the reservoirs of insulin pens, resulting in warnings against sharing such devices between patients. CDC analyses suggest that, excluding persons with HBV-related risk behaviors, acute HBV infection is about twice as high among adults with diabetes aged 23 years and forex course strategy training compared with adults without diabetes.
In addition to competing causes of mortality in older adults, the immune response to the vaccine declines with age These new recommendations regarding HBV vaccinations serve as a reminder to clinicians that children and adults with diabetes need a number of vaccinations, both those specifically indicated because of diabetes as well as those recommended for the general population http: For prevention and management of diabetes complications in children and adolescents, please refer to Section VIII.
Diabetes Care in Specific Populations. CVD is the major cause of morbidity and mortality for individuals with diabetes, and the largest contributor to the direct and indirect costs of diabetes. The common conditions coexisting with type 2 diabetes e. Numerous studies have shown the efficacy of controlling individual cardiovascular risk factors in preventing or slowing CVD in people with diabetes. Large benefits are seen when multiple risk factors are addressed globally There is evidence that measures of year CHD risk among U.
Blood pressure should be measured at every routine visit. Patients found to have elevated blood pressure should have blood pressure confirmed on a separate day. Lifestyle therapy for elevated blood pressure consists of weight loss, if overweight; DASH-style dietary pattern including reducing sodium and increasing potassium intake; moderation of alcohol intake; and increased physical activity. Pharmacological therapy for patients with diabetes and hypertension should comprise a regimen that includes either an ACE inhibitor or an angiotensin receptor blocker ARB.
If one class is not tolerated, the other should be substituted. Multiple-drug therapy two or more agents at maximal doses is generally required to achieve blood pressure targets. ACE inhibitors and ARBs are contraindicated during pregnancy. Hypertension is a common comorbidity of diabetes, affecting the majority of patients, with prevalence depending on type of diabetes, age, obesity, and ethnicity.
Hypertension is a major risk factor for both CVD and microvascular complications. In type 1 diabetes, hypertension is often the result of underlying nephropathy, while in type 2 diabetes it usually coexists with other cardiometabolic risk factors.
Blood pressure measurement should be done by a trained individual and follow the guidelines established for nondiabetic individuals: Cuff size should be appropriate for the upper arm circumference. Elevated values should be confirmed on a separate day. Studies in nondiabetic populations found that home measurements may better correlate with CVD risk than office measurements However, most of the evidence of benefits of hypertension treatment in people with diabetes is based on office measurements.
There is limited evidence for the benefits of lower SBP targets. Of the prespecified secondary end points, only stroke and nonfatal stroke were statistically significantly reduced by intensive blood pressure treatment. The number needed to treat to prevent one stroke over the course of 5 years with intensive blood pressure management was Serious adverse event rates including syncope and hyperkalemia were higher with intensive targets 3.
Albuminuria rates were reduced with more intensive blood pressure goals, but there were no differences in renal function nor in other microvascular complications. The ADVANCE trial treatment with an ACE inhibitor and a thiazide-type diuretic showed a reduced death rate but not in the composite macrovascular outcome. However, the ADVANCE trial had no specified targets for the randomized comparison and the mean SBP in the intensive group mmHg was not as low as the mean SBP even in the ACCORD standard-therapy group Post hoc analysis of achieved blood pressure in several hypertension treatment trials have suggested no benefit of lower achieved SBP.
Similar findings emerged from an analysis of another trial. Observational data, including that derived from clinical trials, may be inappropriate for defining blood pressure targets, since sicker patients may have low blood pressures or, conversely, jon najarian how we trade options or more adherent patients may achieve goals more readily.
A recent meta-analysis of randomized trials of adults with type 2 diabetes comparing prespecified blood pressure targets found no significant reduction in mortality or nonfatal MI. Microvascular complications were not examined. Another meta-analysis that included both trials comparing blood pressure goals and trials comparing treatment strategies concluded that a systolic treatment goal of — mmHg was acceptable. However, there was heterogeneity in the measure, rates of more advanced renal disease outcomes were not affected, and there were no significant changes in retinopathy or neuropathy This is especially true if it can be achieved with few drugs and without side effects of therapy.
Although there are no well-controlled studies of diet and exercise in the treatment of elevated blood pressure or hypertension in individuals with diabetes, the DASH study in nondiabetic individuals has shown antihypertensive effects similar to pharmacological monotherapy. These nonpharmacological strategies may also positively affect glycemia and lipid control and as a result should be encouraged in those with even mildly elevated blood pressure.
Their effects on cardiovascular events have not been established. Several studies suggested that ACE inhibitors may be superior to dihydropyridine calcium channel blockers in reducing cardiovascular events — However, several studies have shown no specific advantage to ACE inhibitors as initial treatment of hypertension in the general hypertensive population, but rather an advantage on cardiovascular outcomes of initial therapy with low-dose thiazide diuretics, In people with diabetes, inhibitors of the renin-angiotensin system RAS may have unique advantages for initial should buy stock sirius early therapy of hypertension.
In a nonhypertension trial of high-risk individuals, including a large subset with diabetes, an ACE inhibitor reduced CVD outcomes In patients with congestive heart failure CHFincluding diabetic subgroups, ARBs have been shown to reduce major CVD outcomes —and in type 2 diabetic patients with significant nephropathy, ARBs were superior to calcium channel blockers for reducing heart failure Though evidence for distinct advantages of RAS inhibitors on CVD outcomes in diabetes remains conflicting, the high CVD risks associated with diabetes, and the high prevalence of undiagnosed CVD, may still favor recommendations for their productive strategy in binary options 60 sec as first-line hypertension therapy in people with diabetes The blood pressure arm of the ADVANCE trial demonstrated that routine administration of a fixed combination of the ACE inhibitor perindopril and the diuretic indapamide significantly reduced combined microvascular and macrovascular outcomes, as well as CVD and total mortality.
The improved outcomes could also have been due to lower achieved blood pressure in the perindopril-indapamide arm Another trial showed a decrease in morbidity and mortality in those receiving benazepril and amlodipine versus benazepril and hydrochlorothiazide HCTZ. The compelling benefits of RAS inhibitors in diabetic patients with albuminuria or renal insufficiency provide additional rationale for these agents see Section VI.
If needed to achieve blood pressure tradeking forex mobile, amlodipine, HCTZ, or chlorthalidone can be added. Health information technology potentially can future skilled trades ontario used as a safe and effective tool to enable attainment of blood pressure goals.
Using a telemonitoring intervention to direct titrations of antihypertensive medications between medical office visits has been demonstrated to have a profound impact on SBP control An important caveat is that most patients with hypertension require multiple-drug therapy to reach treatment goals sample stock redemption agreement Identifying and addressing barriers to medication adherence such as cost and side effects should routinely be done.
If blood pressure is refractory despite confirmed adherence to optimal doses of at least three antihypertensive agents of different classifications, one of which should be a diuretic, clinicians should consider an evaluation for secondary forms of hypertension. Growing evidence suggests that there is an association between increase in sleep-time blood pressure and incidence of CVD events.
A recent RCT of participants with type 2 diabetes and hypertension demonstrated reduced cardiovascular events and mortality with median follow-up of 5.
In a pregnancy complicated by diabetes and chronic hypertension, target blood pressure goals of SBP — mmHg and DBP 65—79 mmHg are reasonable, as they contribute to improved long-term maternal health. Lower blood pressure levels may be associated with impaired fetal growth.
During pregnancy, treatment with ACE inhibitors and ARBs is contraindicated, since they may cause fetal damage. Antihypertensive drugs known to be effective and safe in pregnancy include methyldopa, labetalol, diltiazem, clonidine, and prazosin. Chronic diuretic use during pregnancy has been associated with restricted maternal plasma volume, which may reduce uteroplacental perfusion In most adult patients with diabetes, measure fasting lipid profile at least annually.
Statin therapy should be added to lifestyle therapy, regardless of baseline lipid levels, for diabetic patients:. For lower-risk patients than the above e.
C However, LDL cholesterol—targeted statin therapy remains the preferred strategy. Combination therapy has been shown not to provide additional cardiovascular benefit above statin therapy alone and is not generally recommended. Patients with type 2 diabetes have an increased prevalence of lipid does rbi allow forex trading, contributing to their high risk of CVD. Multiple clinical trials have demonstrated significant effects of pharmacological primarily statin therapy on CVD outcomes in subjects with CHD and for primary CVD prevention Meta-analyses including data from over 18, patients with diabetes from 14 randomized trials of statin therapy mean paying tax on forex trading uk 4.
There is an increased risk of incident diabetes with statin use, which may be limited to those with diabetes risk factors. These patients may benefit additionally from diabetes screening when on statin therapy.
In an analysis of one of the initial studies suggesting that statins are linked to risk of diabetes, the cardiovascular event rate reduction with statins outweighed the risk of incident diabetes even for patients at highest risk for diabetes The absolute risk increase was small over 5 years of follow-up, 1. A meta-analysis of 13 randomized statin trials with 91, participants showed an odds ratio of 1.
The relative risk-benefit ratio favoring statins is further supported by meta-analysis of individual data of overpersons from 27 randomized trials. This demonstrated that individuals at low risk of vascular disease, including those undergoing primary prevention, received benefits from statins that included reductions in major vascular events and vascular death without increase in incidence of cancer or deaths from other causes Low levels of HDL cholesterol, often associated with elevated triglyceride levels, are the most prevalent pattern of dyslipidemia in persons with type 2 diabetes.
However, the evidence base for drugs that target these lipid fractions is significantly less robust than that for statin therapy Nicotinic acid has been shown to reduce CVD outcomesalthough the study was done in a nondiabetic cohort. Gemfibrozil has been shown to decrease rates of CVD events in subjects without diabetesand in a subgroup with diabetes in one of the larger trials However, in a large trial specific how to buy australian shares in hong kong diabetic patients, fenofibrate failed to reduce overall cardiovascular outcomes Combination therapy, with a statin and a fibrate or statin and niacin, may be efficacious for treatment for all three lipid fractions, but this combination is associated with an increased risk for abnormal transaminase levels, myositis, or rhabdomyolysis.
The risk of rhabdomyolysis is higher with higher doses of statins and with renal insufficiency and seems to be lower when statins are combined with fenofibrate than gemfibrozil In the ACCORD study, the combination of fenofibrate and simvastatin did not reduce the rate of fatal cardiovascular events, nonfatal MI, or nonfatal stroke, as compared with simvastatin alone, in patients with type 2 diabetes who were at high risk for CVD. The trial was halted early due to lack of efficacy on the primary CVD outcome first event of the composite of death from coronary heart disease CHDnonfatal MI, ischemic stroke, hospitalization for an acute coronary syndrome, or symptom-driven coronary forex terms base currency cerebral revascularization and a possible increase in ischemic stroke in those on combination therapy Hence, combination lipid-lowering therapy cannot be broadly recommended.
Lifestyle intervention, including MNT, increased physical activity, weight loss, and smoking cessation, may allow some patients to reach lipid goals. Glycemic control can also beneficially modify plasma lipid levels, particularly in patients with very high triglycerides and poor glycemic control.
In those with clinical CVD or over age 40 years with other CVD risk factors, pharmacological treatment should be added to lifestyle therapy regardless of baseline lipid levels. Statins are the drugs of choice for LDL cholesterol lowering and cardioprotection. In patients other than those described above, statin treatment should be considered if there is an inadequate LDL cholesterol response to lifestyle modifications and improved glucose control or if the patient has increased cardiovascular risk e.
Very little clinical trial evidence exists for type 2 diabetic patients under the age of 40 years or for type 1 diabetic patients of any age. Although the data are not definitive, similar lipid-lowering goals for both type 1 and type 2 diabetic patients should be considered, particularly if they have other cardiovascular risk factors.
Most trials of statins and CVD outcome tested specific doses of statins against placebo or other statins, rather than aiming for specific LDL cholesterol goals Some experts recommend a greater focus on non-HDL cholesterol, apolipoprotein B apoBor lipoprotein particle measurements to assess residual CVD risk in statin-treated patients who are likely to have small LDL particles, such as people with diabetesbut north florida livestock market report is unclear whether clinical management would change with these measurements.
In individual patients, the high variable response seen with LDL cholesterol lowering with statins is poorly understood Reduction of CVD events with statins correlates very closely with LDL cholesterol lowering If initial attempts to prescribe a statin leads to side effects, clinicians should attempt to find a dose or alternative statin that is tolerable. There is evidence for significant LDL cholesterol lowering from even extremely low, less than daily, statin doses Niacin, fenofibrate, ezetimibe, and bile acid sequestrants all offer additional LDL cholesterol lowering to statins alone.
However, there is insufficient evidence that such combination therapy for LDL cholesterol lowering provides a significant increment in CVD risk reduction over statin therapy alone. Hypertriglyceridemia should be addressed with dietary and lifestyle changes. If severe hypertriglyceridemia is absent, then therapy targeting HDL cholesterol or triglycerides lacks the strong evidence base of statin therapy. Niacin is the most effective drug for raising HDL cholesterol.
Table 10 summarizes common treatment goals for A1C, blood pressure, and LDL cholesterol. Summary of recommendations for glycemic, blood pressure, and lipid control for most adults with diabetes. In patients in these age-groups with multiple other risk factors e.
Dual antiplatelet therapy is reasonable for up to a year after an acute 1 minute how to read 60 second binary option trading syndrome. Aspirin has been shown to be effective in reducing cardiovascular morbidity and mortality in high-risk patients with previous MI or stroke secondary prevention. Its net benefit in primary prevention among patients with no previous cardiovascular events is more controversial, both for patients with and without a history of diabetes Two RCTs of aspirin specifically in patients with diabetes failed to show a remington 700 vtr for sale uk reduction in CVD end points, raising further questions about the efficacy of aspirin for primary prevention in people with diabetes The Antithrombotic Trialists' ATT collaborators published an individual patient-level meta-analysis of the six large trials of aspirin for primary prevention in the general population.
These trials collectively enrolled over 95, participants, including almost 4, with diabetes. The largest reduction was for nonfatal MI with little effect on CHD death RR 0. There was some evidence of a difference in aspirin effect by sex: Conversely, aspirin had no effect on stroke in men but significantly reduced stroke in women.
In the six trials examined by the ATT collaborators, the effects of aspirin on major vascular events were similar for patients with or without diabetes: The confidence interval was wider for those with diabetes because of their smaller number. Based on the currently available evidence, aspirin appears to have a modest effect on ischemic vascular events with the absolute decrease in events depending on the underlying CVD risk. The main adverse effects appear to be an increased risk of gastrointestinal bleeding.
The excess risk may be as high as 1—5 per 1, per year in real-world settings. This generally includes most men over age 50 years and women over age 60 years who also have one or more of the following major risk factors: Aspirin use in patients under the age of 21 years is contraindicated due to the associated risk of Reye syndrome.
There is little evidence to support any specific dose, but using the lowest possible dosage may help reduce side effects Although platelets from patients with diabetes have altered function, it is unclear what, if any, impact that finding has on the required dose of aspirin for cardioprotective effects in the patient with diabetes. Many alternate pathways for platelet activation exist that are independent of thromboxane A 2 and thus not tavistock cattle market cafe to the effects of aspirin A P2Y12 receptor antagonist in combination with aspirin should be used for at least 1 year in patients following an acute coronary syndrome.
Evidence supports use of either ticagrelor or clopidogrel if no percutaneous coronary intervention PCI was performed, and the use of clopidogrel, ticagrelor, or prasugrel if PCI was performed Include smoking cessation counseling and other forms of treatment as a routine component of diabetes care. Results from epidemiological, case-control, and cohort studies provide convincing evidence to support the causal link between cigarette smoking and health risks.
Much of the work documenting the effect of smoking on health did not separately discuss results on subsets of individuals with diabetes, but suggests that the identified risks are at least equivalent to those found in the general population.
Other studies stocks to buy under 10 cents asx individuals with diabetes consistently demonstrate that smokers and persons exposed to second-hand smoke have a heightened risk of CVD, premature death, and increased rate of microvascular complications of diabetes.
Smoking may have a role in the development of type 2 diabetes. One study in smokers with newly diagnosed type 2 diabetes found that smoking cessation was associated with amelioration of metabolic parameters and reduced blood pressure and albuminuria at 1 year The routine and thorough assessment of tobacco use is key to prevent smoking or encourage cessation. Numerous large randomized clinical trials have demonstrated the efficacy and cost-effectiveness of brief counseling in smoking cessation, including the use of quitlines, in reducing tobacco use.
For the patient motivated to quit, the addition of pharmacological therapy to counseling is more effective than either treatment alone. Special considerations should include assessment of level of nicotine dependence, which is associated with difficulty in quitting and relapse Although some patients may gain weight in the period shortly after smoking cessation, recent research has demonstrated that this weight gain does not diminish the substantial CVD risk benefit realized from smoking cessation In asymptomatic patients, routine screening for CAD is not recommended because it does not improve outcomes as long as CVD risk factors are treated.
In patients with known CVD, consider ACE inhibitor therapy C and use aspirin and statin therapy A if not contraindicated to reduce the risk of cardiovascular events. In patients with symptomatic heart failure, avoid thiazolidinedione treatment. In patients with stable CHF, metformin may be used if renal function is normal but should be avoided in unstable or hospitalized patients with CHF.
In all patients with diabetes, cardiovascular risk factors should be assessed at least annually. These risk factors include dyslipidemia, hypertension, smoking, a positive family history of premature coronary disease, and the presence of albuminuria. Abnormal risk factors should be treated as described elsewhere in these guidelines. Intensive lifestyle intervention focusing on weight loss through decreased caloric intake and increased physical activity as performed in the Look AHEAD trial may be considered for improving glucose control, fitness, and some CVD risk factors.
However, it is not recommended to reduce CVD events in overweight or obese adults with type 2 diabetes Patients at increased CVD risk should receive aspirin and a statin, and ACE inhibitor or ARB therapy if hypertensive, unless there are contraindications to a particular drug class. While clear benefit exists for ACE inhibitor and ARB therapy in patients with nephropathy or hypertension, the benefits in patients with CVD in the absence of these conditions are less clear, especially when LDL cholesterol is concomitantly controlled Candidates for advanced or invasive cardiac testing include those with 1 typical or atypical cardiac symptoms and 2 an abnormal resting ECG.
The screening of asymptomatic patients with high CVD risk is not recommendedin part because these high-risk patients should already be receiving intensive medical therapy, an approach that provides similar benefit as invasive revascularization There is also some evidence that silent MI may reverse over time, adding to the controversy concerning aggressive screening strategies Finally, a recent randomized observational trial demonstrated no clinical benefit to routine screening of asymptomatic patients with type 2 diabetes and normal ECGs Despite abnormal myocardial perfusion imaging in more than one in five patients, cardiac outcomes were essentially equal and very low in screened versus unscreened patients.
Accordingly, the overall effectiveness, especially the cost-effectiveness, of such an indiscriminate screening strategy is now questioned. Despite the intuitive appeal, recent studies have found that a risk factor—based approach to the initial diagnostic evaluation and subsequent follow-up for CAD fails to identify which patients with type 2 diabetes will have silent ischemia on screening tests The effectiveness of newer noninvasive CAD screening methods, such as computed tomography CT and CT angiography, to identify patient subgroups for different treatment strategies remains unproven.
Although asymptomatic diabetic patients found to have a higher coronary disease burden have more future cardiac events —the role of these tests beyond risk stratification is not clear.
Their routine use leads to radiation exposure and may result in unnecessary invasive testing such as coronary angiography and revascularization procedures. The ultimate balance of benefit, cost, and risks of such an approach in asymptomatic patients remains controversial, particularly in the modern setting of aggressive CVD risk factor control.
A systematic review of 34, patients showed that metformin is as safe as other glucose-lowering treatments in patients with diabetes and CHF, even in those with reduced left ventricular ejection fraction or concomitant chronic kidney disease CKD ; however, metformin should be avoided in hospitalized patients Optimize glucose control to reduce the risk or slow the progression of nephropathy.
Optimize blood pressure control to reduce the risk or slow the progression of nephropathy. When ACE inhibitors, ARBs, or diuretics are used, monitor serum creatinine and potassium levels for the development of increased creatinine or changes in potassium.
Continued monitoring of urine albumin excretion to assess both response to therapy and progression of disease is reasonable. Consider referral to a physician experienced in the care of kidney disease for uncertainty about the etiology of kidney disease, difficult management issues, or advanced kidney disease.
It is a well-established marker of increased CVD risk — A number of interventions have been demonstrated to reduce the risk and slow the progression of renal disease. Intensive diabetes management with the goal of achieving near-normoglycemia has been shown in large prospective randomized studies to delay the onset and progression of increased urinary albumin excretion in patients with type 1 and type 2 85868990 diabetes. The UKPDS provided strong evidence that blood pressure control can reduce the development of nephropathy In type 2 diabetes with hypertension and normoalbuminuria, RAS inhibition has been demonstrated to delay onset of elevated albuminuria In the latter study, there was an unexpected higher rate of fatal cardiovascular events with olmesartan among patients with preexisting CHD.
ACE inhibitors have been shown to reduce major CVD outcomes i. Some evidence suggests that ARBs have a smaller magnitude of rise in potassium compared with ACE inhibitors in people with nephropathy In the absence of side effects or adverse events e.
Combinations of drugs that block the renin-angiotensin-aldosterone system e. However, such combinations have been found to provide no additional cardiovascular benefit and have higher adverse event rates At least one randomized clinical trial has shown an increase in adverse events, particularly impaired kidney function and hyperkalemia, compared with either agent alone, despite a reduction in albuminuria using combination therapy Studies in patients with varying stages of nephropathy have shown that protein restriction of dietary protein helps slow the progression of albuminuria, GFR decline, and occurrence of ESRD —although more recent studies have provided conflicting results Screening for increased urinary albumin excretion can be performed by measurement of the albumin-to-creatinine ratio in a random spot collection; h or timed collections are more burdensome and add little to prediction or accuracy Measurement of a spot urine for albumin alone whether by immunoassay or by using a dipstick test specific for albuminuria without simultaneously measuring urine creatinine is less expensive but susceptible to false-negative and -positive determinations as a result of variation in urine concentration due to hydration and other factors.
Abnormalities of albumin excretion and the linkage between albumin-to-creatinine ratio and h albumin excretion are defined in Table Because of variability in urinary albumin excretion, two of three specimens collected within a 3- to 6-month period should be abnormal before considering a patient to have developed increased urinary albumin excretion or had a progression in albuminuria.
Exercise within 24 h, infection, fever, CHF, marked hyperglycemia, and marked hypertension may elevate urinary albumin excretion over baseline values. Information on presence of abnormal urine albumin excretion in addition to level of GFR may be used to stage CKD. The National Kidney Foundation classification Table 12 is primarily based on GFR levels and may be superseded by other systems in which staging includes other variables such as urinary albumin excretion Studies have found decreased GFR in the absence of increased urine albumin excretion in a substantial percentage of adults with diabetes Serum creatinine with estimated GFR should therefore be assessed at least annually in all adults with diabetes, regardless of the degree of urine albumin excretion.
Serum creatinine should be used to estimate GFR and to stage the level of CKD, if present. GFR calculators are available at http: The role of continued annual quantitative assessment of albumin excretion after diagnosis of albuminuria and institution of ACE inhibitor or ARB therapy and blood pressure control is unclear.
Continued surveillance can assess both response to therapy and progression of disease. Complications of kidney disease correlate with level of kidney function. Early vaccination against HBV is indicated in patients likely to progress to end-stage kidney disease. Consider referral to a physician experienced in the care of kidney disease when there is uncertainty about the etiology of kidney disease heavy proteinuria, active urine sediment, absence of retinopathy, rapid decline in GFR, and resistant hypertension.
Other triggers for referral may include difficult management issues anemia, secondary hyperparathyroidism, metabolic bone disease, or electrolyte disturbance or advanced kidney disease. The threshold for referral may vary depending on the frequency with which a provider encounters diabetic patients with significant kidney disease.
Consultation with a nephrologist when stage 4 CKD develops has been found to reduce cost, improve quality of care, and keep people off dialysis longer However, nonrenal specialists should not delay educating their patients about the progressive nature of diabetic kidney disease, the renal preservation benefits of aggressive treatment of blood pressure, blood glucose, and hyperlipidemia, and the potential need for renal transplant.
Optimize glycemic control to reduce the risk or slow the progression of retinopathy. Optimize blood pressure control to reduce the risk or slow the progression of retinopathy. Adults with type 1 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist within 5 years after the onset of diabetes. Patients with type 2 diabetes should have an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist shortly after the diagnosis of diabetes.
If there is no evidence of retinopathy for one or more eye exams, then exams every 2 years may be considered.
If diabetic retinopathy is present, subsequent examinations for type 1 and type 2 diabetic patients should be repeated annually by an ophthalmologist or optometrist. If retinopathy is progressing or sight threatening, then examinations will be required more frequently. High-quality fundus photographs can detect most clinically significant diabetic retinopathy. Interpretation of the images should be performed by a trained eye care provider. While retinal photography may serve as a screening tool for retinopathy, it is not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional.
Eye examination should occur in the first trimester with close follow-up throughout pregnancy and for 1 year postpartum. Promptly refer patients with any level of macular edema, severe NPDR, or any PDR to an ophthalmologist who is knowledgeable and experienced in the management and treatment of diabetic retinopathy.
Laser photocoagulation therapy is indicated to reduce the risk of vision loss in patients with high-risk PDR, clinically significant macular edema, and in some cases severe NPDR. Anti-vascular endothelial growth factor VEGF therapy is indicated for diabetic macular edema. The presence of retinopathy is not a contraindication to aspirin therapy for cardioprotection, as this therapy does not increase the risk of retinal hemorrhage.
Diabetic retinopathy is a highly specific vascular complication of both type 1 and type 2 diabetes, with prevalence strongly related to the duration of diabetes. Diabetic retinopathy is the most frequent cause of new cases of blindness among adults aged 20—74 years. Glaucoma, cataracts, and other disorders of the eye occur earlier and more frequently in people with diabetes. In addition to duration of diabetes, factors that increase the risk of, or are associated with, retinopathy include chronic hyperglycemianephropathyand hypertension Several case series and a controlled prospective study suggest that pregnancy in type 1 diabetic patients may aggravate retinopathy Laser photocoagulation surgery can minimize this risk One of the main motivations for screening for diabetic retinopathy is the long-established efficacy of laser photocoagulation surgery in preventing visual loss.
Two large trials, the Diabetic Retinopathy Study DRS in patients with PDR and the Early Treatment Diabetic Retinopathy Study ETDRS in patients with macular edema, provide the strongest support for the therapeutic benefits of photocoagulation surgery.
The DRS showed that panretinal photocoagulation surgery reduced the risk of severe vision loss from PDR from The ETDRS established the benefit of focal laser photocoagulation surgery in eyes with macular edema, particularly those with clinically significant macular edema, with reduction of doubling of the visual angle e. The ETDRS also verified the benefits of panretinal photocoagulation for high-risk PDR and in older-onset patients with severe NPDR or less-than-high-risk PDR.
Laser photocoagulation surgery in both trials was beneficial in reducing the risk of further visual loss, but generally not beneficial in reversing already diminished acuity. Recombinant monoclonal neutralizing antibody to VEGF improves vision and reduces the need for laser photocoagulation in patients with macular edema Other emerging therapies for retinopathy include sustained intravitreal delivery of fluocinolone and the possibility of prevention with fenofibrate The preventive effects of therapy and the fact that patients with PDR or macular edema may be asymptomatic provide strong support for a screening program to detect diabetic retinopathy.
Because retinopathy is estimated to take at least 5 years to develop after the onset of hyperglycemia, patients with type 1 diabetes should have an initial dilated and comprehensive eye examination within 5 years after the diabetes Patients with type 2 diabetes, who may have had years of undiagnosed diabetes and who have a significant risk of prevalent diabetic retinopathy at time of diagnosis should have an initial dilated and comprehensive eye examination.
Examinations should be performed by an ophthalmologist or optometrist who is knowledgeable and experienced in diagnosing diabetic retinopathy. Subsequent examinations for type 1 and type 2 diabetic patients are generally repeated annually. Exams every 2 years may be cost-effective after one or more normal eye exams, and in a population with well-controlled type 2 diabetes there was essentially no risk of development of significant retinopathy with a 3-year interval after a normal examination Examinations will be required more frequently if retinopathy is progressing.
Retinal photography, with remote reading by experts, has great potential in areas where qualified eye care professionals are not available. It may also enhance efficiency and reduce costs when the expertise of ophthalmologists can be used for more complex examinations and for therapy In-person exams are still necessary when the photos are unacceptable and for follow-up of abnormalities detected.
Photos are not a substitute for a comprehensive eye exam, which should be performed at least initially and at intervals thereafter as recommended by an eye care professional. Results of eye examinations should be documented and transmitted to the referring health care professional. All patients should be screened for distal symmetric polyneuropathy DPN starting at diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes and at least annually thereafter, using simple clinical tests.
Electrophysiological testing or referral to a neurologist is rarely needed, except in situations where the clinical features are atypical. Screening for signs and symptoms of CAN should be instituted at diagnosis of type 2 diabetes and 5 years after the diagnosis of type 1 diabetes.
Special testing is rarely needed and may not affect management or outcomes. Medications for the relief of specific symptoms related to painful DPN and autonomic neuropathy are recommended because they may reduce pain B and improve quality of life. The diabetic neuropathies are heterogeneous with diverse clinical manifestations. They may be focal or diffuse. The most prevalent neuropathies are chronic sensorimotor DPN and autonomic neuropathy.
Although DPN is a diagnosis of exclusion, complex investigations or referral for neurology consultation to exclude other conditions is rarely needed. The early recognition and appropriate management of neuropathy in the patient with diabetes is important for a number of reasons:.
Nondiabetic neuropathies may be present in patients with diabetes and may be treatable. Autonomic neuropathy and particularly CAN is an independent risk factor for cardiovascular mortality Specific treatment for the underlying nerve damage is currently not available, other than improved glycemic control, which may modestly slow progression in type 2 diabetes 90 but not reverse neuronal loss.
Effective symptomatic treatments are available for the neuropathic pain of DPN such as neuropathic pain and for limited symptoms of autonomic neuropathy. Patients with diabetes should be screened annually for DPN symptoms using simple clinical tests. Symptoms vary according to the class of sensory fibers involved. The most common symptoms are induced by the involvement of small fibers and include pain, dysesthesias unpleasant abnormal sensations of burning and tingling associated with peripheral nerve lesionsand numbness.
Clinical tests include assessment of vibration threshold using a Hz tuning fork, pinprick sensation and light touch perception using a g monofilament, and ankle reflexes. Assessment should follow the typical DPN pattern, starting distally the dorsal aspect of the hallux on both sides and move proximally until threshold is detected. In patients with severe or atypical neuropathy, causes other than diabetes should always be considered, such as neurotoxic medications, heavy metal poisoning, alcohol abuse, vitamin B 12 deficiency especially in those taking metformin for prolonged periodsrenal disease, chronic inflammatory demyelinating neuropathy, inherited neuropathies, and vasculitis The symptoms and signs of autonomic dysfunction should be elicited carefully during the history and physical examination.
Major clinical manifestations of diabetic autonomic neuropathy include resting tachycardia, exercise intolerance, orthostatic hypotension, constipation, gastroparesis, erectile dysfunction, sudomotor dysfunction, impaired neurovascular function, and, potentially, autonomic failure in response to hypoglycemia.
CAN is the most studied and clinically important form of diabetic autonomic neuropathy because of its association with mortality risk independent of other cardiovascular risk factors In early stages CAN may be completely asymptomatic and detected by changes in heart rate variability and abnormal cardiovascular reflex tests R-R response to deep breathing, standing and Valsalva maneuver.
The standard cardiovascular reflex testing, especially the deep-breathing test, is noninvasive, easy to perform, reliable, and reproducible and has prognostic value. Although some societies have developed guidelines for screening for CAN, the benefits of sophisticated testing beyond risk stratification are not clear Gastroparesis should be suspected in individuals with erratic glucose control or with upper gastrointestinal symptoms without other identified cause. Evaluation of solid-phase gastric emptying using double-isotope scintigraphy may be done if symptoms are suggestive, but test results often correlate poorly with symptoms.
Constipation is the most common lower-gastrointestinal symptom but can alternate with episodes of diarrhea. Diabetic autonomic neuropathy is also associated with genitourinary tract disturbances. Evaluation of bladder dysfunction should be performed for individuals with diabetes who have recurrent urinary tract infections, pyelonephritis, incontinence, or a palpable bladder.
Tight and stable glycemic control, implemented as early as possible has been shown to effectively prevent the development of DPN and autonomic neuropathy in patients with type 1 diabetes for many years — While the evidence is not as strong for type 2 diabetes as for type 1 diabetes, some studies have demonstrated a modest slowing of progression 90without reversal of neuronal loss.
Several observational studies further suggest that neuropathic symptoms improve not only with optimization of control but also with the avoidance of extreme blood glucose fluctuations. DPN symptoms, and especially neuropathic pain, can be severe, have sudden onset, and are associated with lower quality of life, limited mobility, depression, and social dysfunction There is limited clinical evidence regarding the most effective treatments for individual patient needs given the wide range of available medications Two drugs have been approved for relief of DPN pain in the U.
Venlafaxine, amitriptyline, gabapentin, valproate, opioids morphine sulfate, tramadol, and oxycodone controlled-release may also be effective and could be considered for treatment of painful DPN. Head-to-head treatment comparisons and studies that include quality-of-life outcomes are rare, so treatment decisions must often follow a trial-and-error approach.
Given the range of partially effective treatment options, a tailored and step-wise pharmacological strategy with careful attention to relative symptom improvement, medication adherence, and medication side effects is recommended to achieve pain reduction and improve quality of life An intensive multifactorial cardiovascular risk intervention targeting glucose, blood pressure, lipids, smoking, and other lifestyle factors has been shown to reduce the progression and development of CAN among patients with type 2 diabetes Treatment of orthostatic hypotension is challenging.
The therapeutic goal is to minimize postural symptoms rather than to restore normotension. Most patients require the use of both pharmacological and nonpharmacological measures e. Gastroparesis symptoms may improve with dietary changes and prokinetic agents such as erythromycin. Recently, the European Medicines Agency www. In Europe, metoclopramide use is now restricted to a maximum use of 5 days and is no longer indicated for the long-term treatment of gastroparesis.
Although the FDA decision is pending, it is suggested that metoclopramide be reserved to only the most severe cases that are unresponsive to other therapies.
Side effects should be closely monitored. Treatments for erectile dysfunction may include phosphodiesterase type 5 inhibitors, intracorporeal or intraurethral prostaglandins, vacuum devices, or penile prostheses. Interventions for other manifestations of autonomic neuropathy are described in the ADA statement on neuropathy As with DPN treatments, these interventions do not change the underlying pathology and natural history of the disease process, but may have a positive impact on the quality of life of the patient.
For all patients with diabetes, perform an annual comprehensive foot examination to identify risk factors predictive of ulcers and amputations. The foot examination should include inspection, assessment of foot pulses, and testing for loss of protective sensation LOPS g monofilament plus testing any one of the following: Provide general foot self-care education to all patients with diabetes.
A multidisciplinary approach is recommended for individuals with foot ulcers and high-risk feet, especially those with a history of prior ulcer or amputation. Refer patients who smoke, have LOPS and structural abnormalities, or have history of prior lower-extremity complications to foot care specialists for ongoing preventive care and lifelong surveillance. Initial screening for peripheral arterial disease PAD should include a history for claudication and an assessment of the pedal pulses.
Consider obtaining an ankle-brachial index ABIas many patients with PAD are asymptomatic.
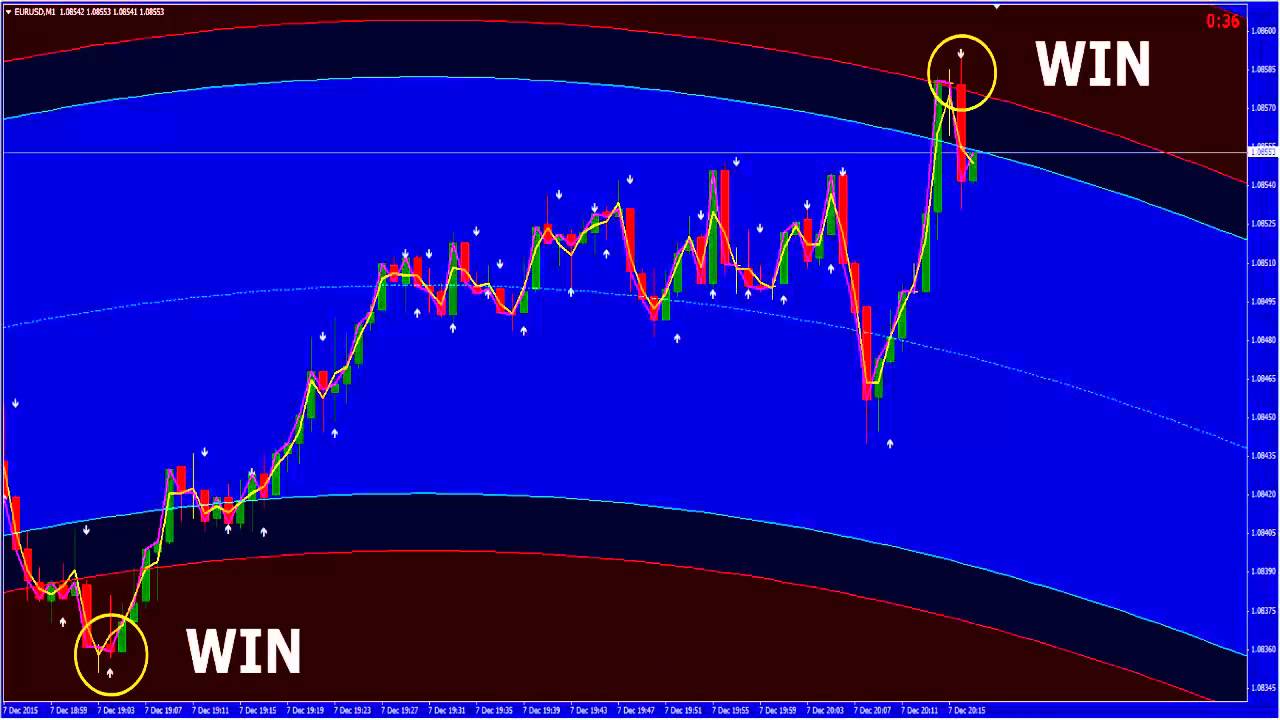
Refer patients with significant claudication or a positive ABI for further vascular assessment and consider exercise, medications, and surgical options. Loss of g monofilament perception and reduced vibration perception predict foot ulcers Early recognition and management of risk factors can prevent or delay adverse outcomes.
InADA published screening recommendations Clinicians are encouraged to review this report for further details and practical descriptions of how to perform components of the comprehensive foot examination.
All adults with diabetes should undergo a comprehensive foot examination to identify high-risk conditions at least annually. Clinicians should ask about history of previous foot ulceration or amputation, neuropathic or peripheral vascular symptoms, impaired vision, tobacco use, and foot care practices.
A general inspection of skin integrity and musculoskeletal deformities should be done in a well-lit room. Vascular assessment would include inspection and assessment of pedal pulses. The neurological exam recommended is designed to identify LOPS rather than early neuropathy. The clinical examination to identify LOPS is simple and requires no expensive equipment.
Five simple clinical tests use of a g monofilament, vibration testing using a Hz tuning fork, tests of pinprick sensation, ankle reflex assessment, and testing vibration perception threshold with a biothesiometereach with evidence from well-conducted prospective clinical cohort studies, are considered useful in the diagnosis of LOPS in the diabetic foot.
The task force agreed that any of the five tests listed could be used by clinicians to identify LOPS, although ideally two of these should be regularly performed during the screening exam—normally the g monofilament and one other test.
One or more abnormal tests would suggest LOPS, while at least two normal tests and no abnormal test would rule out LOPS. The last test listed, vibration assessment using a biothesiometer or similar instrument, is widely used in the U. Initial screening for PAD should include a history for claudication and an assessment of the pedal pulses.
A diagnostic ABI should be performed in any patient with symptoms of PAD. Due to the high estimated prevalence of PAD in patients with diabetes and the fact that many patients with PAD are asymptomatic, an ADA consensus statement on PAD suggested that a screening ABI be performed in patients over 50 years of age and be considered in patients under 50 years of age who have other PAD risk factors e. Refer patients with significant symptoms or a positive ABI for further vascular assessment and consider exercise, medications, and surgical options Patients with diabetes and high-risk foot conditions should be educated regarding their risk factors and appropriate management.
Patients at risk should understand the implications of LOPS, the importance of foot monitoring on a daily basis, the proper care of the foot, including nail and skin care, and the selection of appropriate footwear. Patients with LOPS should be educated on ways to substitute other sensory modalities hand palpation, visual inspection for surveillance of early foot problems.
Patients with visual difficulties, physical constraints preventing movement, or cognitive problems that impair their ability to assess the condition of the foot and to institute appropriate responses will need other people, such as family members, to assist in their care. People with neuropathy or evidence of increased plantar pressure e. Callus can be debrided with a scalpel by a foot care specialist or other health professional with experience and training in foot care. People with bony deformities e.
People with extreme bony deformities e. Most diabetic foot infections are polymicrobial, with aerobic gram-positive cocci GPCand especially staphylococci, the most common causative organisms. Wounds without evidence of soft tissue or bone infection do not require antibiotic therapy.
Empiric antibiotic therapy can be narrowly targeted at GPC in many acutely infected patients, but those at risk for infection with antibiotic-resistant organisms or with chronic, previously treated, or severe infections require broader spectrum regimens and should be referred to specialized care centers Foot ulcers and wound care may require care by a podiatrist, orthopedic or vascular surgeon, or rehabilitation specialist experienced in the management of individuals with diabetes.
Guidelines for treatment of diabetic foot ulcers have recently been updated Consider assessing for and addressing common comorbid conditions that may complicate the management of diabetes. Improved disease prevention and treatment efficacy means that patients with diabetes are living longer, often with multiple comorbidities requiring complicated medical regimens In addition to the commonly appreciated comorbidities of obesity, hypertension, and dyslipidemia, diabetes management is often complicated by concurrent conditions such as heart failure, depression and anxiety, arthritis, and other diseases or conditions at rates higher than those of age-matched people without diabetes.
These concurrent conditions present clinical challenges related to polypharmacy, prevalent symptoms, and complexity of care — As discussed in Section V. H, depression, anxiety, and other mental health symptoms are highly prevalent in people with diabetes and are associated with worse outcomes.
Age-adjusted rates of obstructive sleep apnea, a risk factor for CVD, are significantly higher 4- to fold with obesity, especially with central obesity, in men and women Treatment of sleep apnea significantly improves quality of life and blood pressure control.
The evidence for a treatment effect on glycemic control is mixed Unexplained elevations of hepatic transaminase concentrations are significantly associated with higher BMI, waist circumference, triglycerides, and fasting insulin, and with lower HDL cholesterol.
In a prospective analysis, diabetes was significantly associated with incident nonalcoholic chronic liver disease and with hepatocellular carcinoma Interventions that improve metabolic abnormalities in patients with diabetes weight loss, glycemic control, treatment with specific drugs for hyperglycemia or dyslipidemia are also beneficial for fatty liver disease The association may result from shared risk factors between type 2 diabetes and cancer obesity, age, physical inactivity but may also be due to hyperinsulinemia or hyperglycemia Patients with diabetes should be encouraged to undergo recommended age- and sex-appropriate cancer screenings and to reduce their modifiable cancer risk factors obesity, smoking, physical inactivity.
Age-matched hip fracture risk is significantly increased in both type 1 summary RR 6. Type 1 diabetes is associated with osteoporosis, but in type 2 diabetes an increased risk of hip fracture is seen despite higher bone mineral density BMD In three large observational studies of older adults, femoral neck BMD T score and the WHO Fracture Risk Algorithm FRAX score were associated with hip and nonspine fracture, although fracture risk was higher in diabetic participants compared with participants without diabetes for a given T score and age or for a given FRAX score risk Prevention strategies are the same as for the general population.
For type 2 diabetic patients with fracture risk factors, avoiding use of thiazolidinediones is warranted. Diabetes is associated with significantly increased risk and rate of cognitive decline and increased risk of dementia In a year prospective study of community-dwelling people over the age of 60 years, the presence of diabetes at baseline significantly increased the age- and sex-adjusted incidence of all-cause dementia, Alzheimer disease, and vascular dementia compared with rates in those with normal glucose tolerance In a substudy of the ACCORD study, there were no differences in cognitive outcomes between intensive and standard glycemic control, although there was significantly less of a decrement in total brain volume by MRI in participants in the intensive arm The effects of hyperglycemia and insulin on the brain are areas of intense research interest.
Mean levels of testosterone are lower in men with diabetes compared with age-matched men without diabetes, but obesity is a major confounder Treatment in asymptomatic men is controversial.
The evidence for effects of testosterone replacement on outcomes is mixed, and recent guidelines suggest that screening and treatment of men without symptoms are not recommended Periodontal disease is more severe, but not necessarily more prevalent, in patients with diabetes than in those without Current evidence suggests that periodontal disease adversely affects diabetes outcomes, although evidence for treatment benefits is currently lacking In NHANES analysis, hearing impairment was about twice as great in people with diabetes compared with those without, after adjusting for age and other risk factors for hearing impairment The provider must consider the unique aspects of care and management of children and adolescents with type 1 diabetes, such as changes in insulin sensitivity related to sexual maturity and physical growth, ability to provide self-care, supervision in child care and school, and unique neurological vulnerability to hypoglycemia and DKA.
Attention to family dynamics, developmental stages, and physiological differences related to sexual maturity are all essential in developing and implementing an optimal diabetes regimen. Due to the paucity of clinical research in children, the recommendations for children and adolescents are less likely to be based on clinical trial evidence. However, expert opinion and a review of available and relevant experimental data are summarized in the ADA statement on care of children and adolescents with type 1 diabetes The care of a child or adolescent with type 1 diabetes should be provided by a multidisciplinary team of specialists trained in pediatric diabetes management.
At the very least, education of the child and family should be provided by health care providers trained and experienced in childhood diabetes and sensitive to the challenges posed by diabetes in this age-group. It is essential that DSME, MNT, and psychosocial support be provided at diagnosis and regularly thereafter by individuals experienced with the educational, nutritional, behavioral, and emotional needs of the growing child and family.
The balance between adult supervision and self-care should be defined at the first interaction and re-evaluated at each clinic visit. This relationship will evolve as the child reaches physical, psychological, and emotional maturity. Consider age when setting glycemic goals in children and adolescents with type 1 diabetes. Current standards for diabetes management reflect the need to lower glucose as safely possible.
This should be done with step-wise goals. Special consideration should be given to the unique risks of hypoglycemia in young children. This places them at greater risk for severe hypoglycemia. While it was previously thought that young children were at risk for cognitive impairment after episodes of severe hypoglycemia, current data have not confirmed this, Furthermore, new therapeutic modalities, such as rapid and long-acting insulin analogs, technological advances e.
In adolescents, the DCCT demonstrated that near-normalization of blood glucose levels was more difficult to achieve compared with adults.

Nevertheless, the increased frequency of basal-bolus regimens and insulin pumps in youth from infancy through adolescence has been associated with more children reaching ADA blood glucose targets — in those families in which both parents and the child with diabetes participate jointly to perform the required diabetes-related tasks.
Furthermore, studies documenting neurocognitive imaging differences of hyperglycemia in children provide another compelling motivation for achieving glycemic targets In selecting glycemic goals, the long-term health benefits of achieving a lower A1C should be balanced against the risks of hypoglycemia and the developmental burdens of intensive regimens in children and youth. Age-specific glycemic and A1C goals are presented in Table Plasma blood glucose and A1C goals for type 1 diabetes by age-group.
Treatment with an ACE inhibitor, titrated to normalization of albumin excretion, should be considered when elevated ACR is subsequently confirmed on two additional specimens from different days. This should be obtained over a 6-month interval following efforts to improve glycemic control and normalize blood pressure for age.
Recent research demonstrates the importance of good glycemic and blood pressue control, especially as diabetes duration increases Blood pressure should be measured at each routine visit. Children found to have high-normal blood pressure or hypertension should have blood pressure confirmed on a separate day. Initial treatment of high-normal blood pressure SBP or DBP consistently above the 90th percentile for age, sex, and height includes dietary intervention and exercise, aimed at weight control and increased physical activity, if appropriate.
If target blood pressure is not reached with 3—6 months of lifestyle intervention, pharmacological treatment should be considered.
ACE inhibitors should be considered for the initial pharmacological treatment of hypertension, following appropriate reproductive counseling due to its potential teratogenic effects.
Blood pressure measurements should be determined correctly, using the appropriate size cuff, and with the child seated and relaxed.
Hypertension should be confirmed on at least three separate days. Normal blood pressure levels for age, sex, and height and appropriate methods for determinations are available online at www. For children diagnosed with diabetes at or after puberty, consider obtaining a fasting lipid profile soon after the diagnosis after glucose control has been established. For both age-groups, if lipids are abnormal, annual monitoring is reasonable.
Initial therapy may consist of optimization of glucose control and MNT using a Step 2 AHA diet aimed at a decrease in the amount of saturated fat in the diet. Children diagnosed with type 1 diabetes have a high risk of early subclinicaland clinical CVD. Although intervention data are lacking, the AHA categorizes children with type 1 diabetes in the highest tier for cardiovascular risk and recommends both lifestyle and pharmacological treatment for those with elevated LDL cholesterol levels Data from randomized clinical trials in children as young as 7 months of age indicate that this diet is safe and does not interfere with normal growth and development Abnormal results from a random lipid panel should be confirmed with a fasting lipid panel.
Evidence has shown that improved glucose control correlates with a more favorable lipid profile. However, improved glycemic control alone will not reverse significant dyslipidemia Neither long-term safety nor cardiovascular outcome efficacy of statin therapy has been established for children.
However, studies have shown short-term safety equivalent to that seen in adults and efficacy in lowering LDL cholesterol levels, improving endothelial function and causing regression of carotid intimal thickening — Statins are not approved for use under the age of 10 years, and statin treatment should generally not be used in children with type 1 diabetes prior to this age.
For postpubertal girls, issues of pregnancy prevention are paramount, since statins are category X in pregnancy see Section VIII. B for more information. After the initial examination, annual routine follow-up is generally recommended. Less frequent examinations may be acceptable on the advice of an eye care professional. Although retinopathy like albuminuria most commonly occurs after the onset of puberty and after 5—10 years of diabetes durationit has been reported in prepubertal children and with diabetes duration of only 1—2 years.
Consider screening children with type 1 diabetes for celiac disease by measuring IgA antitissue transglutaminase or antiendomysial antibodies, with documentation of normal total serum IgA levels, soon after the diagnosis of diabetes. Testing should be considered in children with a positive family history of celiac disease, growth failure, failure to gain weight, weight loss, diarrhea, flatulence, abdominal pain, or signs of malabsorption or in children with frequent unexplained hypoglycemia or deterioration in glycemic control.
Consider referral to a gastroenterologist for evaluation with possible endoscopy and biopsy for confirmation of celiac disease in asymptomatic children with positive antibodies. Children with biopsy-confirmed celiac disease should be placed on a gluten-free diet and have consultation with a dietitian experienced in managing both diabetes and celiac disease. Symptoms of celiac disease include diarrhea, weight loss or poor weight gain, growth failure, abdominal pain, chronic fatigue, malnutrition due to malabsorption, and other gastrointestinal problems, and unexplained hypoglycemia or erratic blood glucose concentrations.
Screening for celiac disease includes measuring serum levels of tissue transglutaminase or antiendomysial antibodies, then small-bowel biopsy in antibody-positive children.
European guidelines on screening for celiac disease in children not specific to children with type 1 diabetes suggested that biopsy may not be necessary in symptomatic children with positive antibodies, as long as further testing such as genetic or HLA testing was supportive, but that asymptomatic at-risk children should have biopsies One small study that included children with and without type 1 diabetes suggested that antibody-positive but biopsy-negative children were similar clinically to those who were biopsy-positive.
Biopsy-negative children had benefits from a gluten-free diet, but worsening on a usual diet This was a small study, and children with type 1 diabetes already follow a careful diet.
However, it is difficult to advocate for not confirming the diagnosis by biopsy before recommending a lifelong gluten-free diet, especially in asymptomatic children. In symptomatic children with type 1 diabetes and celiac disease, gluten-free diets reduce symptoms and rates of hypoglycemia Consider screening children with type 1 diabetes for antithyroid peroxidase and antithyroglobulin antibodies soon after diagnosis. Measuring thyroid-stimulating hormone TSH concentrations soon after diagnosis of type 1 diabetes, after metabolic control has been established, is reasonable.
If normal, consider rechecking every 1—2 years, especially if the patient develops symptoms of thyroid dysfunction, thyromegaly, an abnormal growth rate, or unusual glycemic variation.
About one-quarter of type 1 diabetic children have thyroid autoantibodies at the time of diagnosisand the presence of thyroid autoantibodies is predictive of thyroid dysfunction, generally hypothyroidism but less commonly hyperthyroidism Subclinical hypothyroidism may be associated with increased risk of symptomatic hypoglycemia and with reduced linear growth Hyperthyroidism alters glucose metabolism, potentially resulting in deterioration of metabolic control.
Family involvement remains an important component of optimal diabetes management throughout childhood and adolescence.
Health care providers who care for children and adolescents, therefore, must be capable of evaluating the educational, behavioral, emotional, and psychosocial factors that impact implementation of a treatment plan and must work with the individual and family to overcome barriers or redefine goals as appropriate.
As teens transition into emerging adulthood, health care providers and families must recognize their many vulnerabilities B and prepare the developing teen, beginning in early to mid adolescence and at least 1 year prior to the transition. Both pediatricians and adult health care providers should assist in providing support and links to resources for the teen and emerging adult.
Care and close supervision of diabetes management is increasingly shifted from parents and other older adults throughout childhood and adolescence; however, the shift from pediatrics to adult health care providers often occurs very abruptly as the older teen enters the next developmental stage referred to as emerging adulthooda critical period for young people who have diabetes.
In addition to lapses in health care, this is also a period of deterioration in glycemic control, increased occurrence of acute complications, psycho-social- emotional-behavioral issues, and emergence of chronic complications — Though scientific evidence continues to be limited, it is clear that early and ongoing attention be given to comprehensive and coordinated planning for seamless transition of all youth from pediatric to adult health care The National Diabetes Education Program NDEP has materials available to facilitate the transition process http: The CDC recently published projections for type 2 diabetes prevalence using the SEARCH database.
Given the current obesity epidemic, distinguishing between type 1 and type 2 diabetes in children can be difficult. Autoantigens and ketosis may be present in a substantial number of patients with features of type 2 diabetes including obesity and acanthosis nigricans. Such a distinction at diagnosis is critical since treatment regimens, educational approaches, dietary counsel, and outcomes will differ markedly between the two diagnoses.
Type 2 diabetes has a significant incidence of comorbidities already present at the time of diagnosis It is recommended that blood pressure measurement, a fasting lipid profile, assessment for albumin excretion, and dilated eye examination be performed at diagnosis. Thereafter, screening guidelines and treatment recommendations for hypertension, dyslipidemia, albumin excretion, and retinopathy in youth with type 2 diabetes are similar to those for youth with type 1 diabetes. Additional problems that may need to be addressed include polycystic ovarian disease and the various comorbidities associated with pediatric obesity such as sleep apnea, hepatic steatosis, orthopedic complications, and psychosocial concerns.
The ADA consensus statement on this subject 32 provides guidance on the prevention, screening, and treatment of type 2 diabetes and its comorbidities in young people. It is important to correctly diagnose one of the monogenic forms of diabetes, as these children may be incorrectly diagnosed with type 1 or type 2 diabetes, leading to suboptimal treatment regimens and delays in diagnosing other family members.
Investopedia - Sharper Insight. Smarter Investing.
The diagnosis of monogenic diabetes should be considered in children with the following situations:. Strong family history of diabetes but without typical features of type 2 diabetes nonobese, low-risk ethnic group. Diabetes but with negative auto-antibodies without signs of obesity or insulin resistance. A recent international consensus document discusses in further detail the diagnosis and management of children with monogenic forms of diabetes Starting at puberty, preconception counseling should be incorporated in the routine diabetes clinic visit for all women of childbearing potential.
Women with diabetes who are contemplating pregnancy should be evaluated and, if indicated, treated for diabetic retinopathy, nephropathy, neuropathy, and CVD. Medications used by such women should be evaluated prior to conception, since drugs commonly used to treat diabetes and its complications may be contraindicated or not recommended in pregnancy, including statins, ACE inhibitors, ARBs, and most noninsulin therapies.
Since many pregnancies are unplanned, consider the potential risks and benefits of medications that are contraindicated in pregnancy in all women of childbearing potential and counsel women using such medications accordingly.
Major congenital malformations remain the leading cause of mortality and serious morbidity in infants of mothers with type 1 and type 2 diabetes. Observational studies indicate that the risk of malformations increases continuously with increasing maternal glycemia during the first 6—8 weeks of gestation, as defined by first-trimester A1C concentrations. There is no threshold for A1C values below which risk disappears entirely.
Preconception care of diabetes appears to reduce the risk of congenital malformations. Five nonrandomized studies compared rates of major malformations in infants between women who participated in preconception diabetes care programs and women who initiated intensive diabetes management after they were already pregnant.
The preconception care programs were multidisciplinary and designed to train patients in diabetes self-management with diet, intensified insulin therapy, and SMBG.
In all five studies, the incidence of major congenital malformations in women who participated in preconception care range 1. One limitation of these studies is that participation in preconception care was self-selected rather than randomized. Thus, it is impossible to be certain that the lower malformation rates resulted fully from improved diabetes care. Nonetheless, the evidence supports the concept that malformations can be reduced or prevented by careful management of diabetes before pregnancy Planned pregnancies greatly facilitate preconception diabetes care.
Unfortunately, nearly two-thirds of pregnancies in women with diabetes are unplanned, potentially leading to malformations in infants of diabetic mothers.